Digital Triage and Demand-Flow. EFPC Porto
Hypothesis: efficient operation of primary care depends on clinical triage of all demand, to optimise the use of scarce consulting resource – GP time.
The faster and simpler the system, the more patients will co-operate.
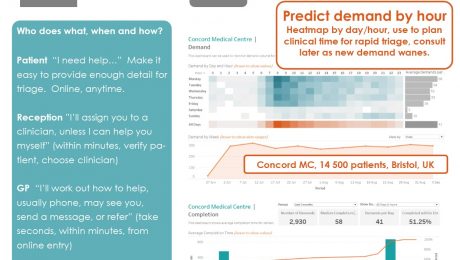
Who does what, when and how?
Patient “I need help…” Make it easy to provide enough detail for triage. Online, anytime.
Reception ”I’ll assign you to a clinician, unless I can help you myself” (within minutes, verify patient, choose clinician)
GP “I’ll work out how to help, usually phone, may see you, send a message, or refer” (take seconds, within minutes, from online entry)
Consult & complete – precisely appropriate for the patient and episode.
Presented at EFPC European Forum for Primary Care, Annual Conference Porto 24-26 September 2017
Download the poster here:
- Published in Evidence
Bad general practice is driving out good
Known since before Tudor times, named Gresham’s law in 1860, thoughtful observers have realised that “Bad money drives out good”. When two forms of currency are in circulation, the debased version quickly replaces that of true value. It’s happening now, paid for by the NHS, in general practice.
Oxford CCG proudly trumpets the big numbers, “15,000 extra GP appointments in £4m scheme.” Divide £4m by 15,000 x 12 months and we find the cost per appointment is £67. That’s over twice the fully absorbed average cost of a regular GP appointment.
It gets worse: regular GPs are funded by capitation, not by activity (per appointment) and their contract means they are already responsible for their registered patients who are or believe themselves to be ill. The CCG is paying £6 per patient for a service already fully funded – it’s paying twice. But not the CCG – it comes from an NHS England pot, descended from a GP Access fund which covered less than 10% of England – a lottery as to whether your area is included.
It gets worse: a GP federation officer says it’s for those patients having to wait 2 to 3 weeks to see their own GP. These GPs are failing their patients with an appalling service. They are being rewarded for failure, incentivised to fail more as worse access will move more of their patients into the “extended service hubs”. Patients at GPs offering an excellent service, such as Oak Tree Didcot which we helped over 5 years ago, have no need and no desire to travel further to see a doctor they don’t know.
It gets worse: my Didcot GP friend tells me “it is virtually impossible to find GP locums or recruit GPs because many are now working in these hubs seeing relatively straight forward problems, with 15 minute appointments, whether the patient needs 15 minutes or not.” [and we know that utilisation of slots is low, many will be left empty]
All right thinking people can see this. So why is it happening? Control of the money lies with those who don’t want to see: NHS England, who knows why, Oxford CCG who think they have a “nice” headline, and the GP federation owners so happy to take up the offer of highly profitable light duties. £4m will get soaked up in a year with no difficulty at all, and when the money stops, so will the service. This is the very antithesis of sustainable continuous improvement.
What can you do? Fight this debasing of general practice with every bone in your body. The RCGP, BMA and all in leadership positions should be calling this out. Local GP Dr Helen Salisbury says, “It might be better if we could just fund GPs properly,’ Too right. NHS funding must go to where it is of highest quality, most effective and productive, core general practice.
I don’t like to end without hope, because we need hope, and Gregory Bateson’s analogue is worth noting: “the oversimplified ideas will always displace the sophisticated, and the vulgar and hateful will always displace the beautiful. And yet the beautiful persists.”
Fight for the beautiful.
Harry Longman
PS last week’s launch in Surrey has gone well, GPs dealing with all demand on the day, patients amazed. A couple of examples stood out for me on day one: the lady who walked straight to the desk at 8:35 expecting a queue of 10 and a rammed waiting room: nobody. Look of total bewilderment – “are you open?” And the patient late in the afternoon who, on the way out, stopped at reception to thank the whole team for the wonderful service she’d had. Gets me out of bed every morning.
- Published in Comment
Fancy a 10 hour working day?
I do hope you are thoroughly refreshed and have enjoyed the break from my blog. I mean your work. Oh, whatever, I’ll stop digging.
But I wonder how you view the thought of a 10 hour working day? Horror or relief? It’s relative isn’t it, because to some that would be 2.5 hours over the regulation 7.5, to others it might bring sanity at last to a regime which has been 12 or even 14 hours. People aren’t made for that and whatever you earn, it can make life not worth living.
So I was struck when a GP partner recently said she had this burning ambition for a 10 hour day, when completing our Could you be ready to change? (we do this with everyone thinking about system change. Nothing matters more than having a burning ambition).
Reducing GP workload has been number one topic in Pulse, BMA, RCGP and goodness knows where else, and the bad news is that we can’t wave a magic wand to reduce it. There are lots of factors. One is patient demand, which is remarkably constant, whatever we do. It isn’t going up, though revisiting a Liverpool practice we first helped five years ago is encouraging – demand is down 10%.
But what we can do, and to some this does seem like a miracle, is dramatically improve efficiency. It’s intense, and getting it right means careful analysis of consultation times, modes, referral and resolve rates, but it does work. Unmet demand is a factor, and simply meeting this can soak up a proportion of time freed up by a 20% efficiency gain, but almost always there’s plenty left over for getting the hours down.
Efficiency is our absolute laser focus – how you convert that to your benefit is up to you.
Overwhelmingly GPs tell us “I feel more in control”, as another partner did last month having launched in June, and it’s the control that makes work satisfying, even though it can be intense.
We love what we do and those kind of comments get me out of bed every morning. It will be an early start Monday to be at our first autumn launch in Surrey – I can hardly wait.
Harry Longman
- Published in Comment