GPAD data submissions to NHS England
This note is to update users on data submissions to NHS England for activity reporting.
You may know that practices are required to submit activity data from 30 June 2021 as outlined on their website here.
Many practices made representations that this would create extra work for no benefit, as many patient requests are completed with no need for an “appointment” record.
We have seen a copy of a post on the forum “FutureNHS” by “Digital First Primary Care”
We are raising this with system suppliers with the aim to gather that data directly from them. If a Practice has started / or is happy to map across both systems, this would ultimately create a better reporting data and Practices can continue to do this.
However, if this is not currently being recorded in the GP Clinical system appointment book, the current advice is not to double record in the GP Clinical System appointment book due to the extra burden on Practices.
When the data is published it will include a caveat highlighting that the GP appointment book is not the only tool which captures appointments and for those appointments captured elsewhere we have not got the means of capturing that data.
We have requested an official communication to this effect but have had no reply so far.
The message seems to be a positive one, there is no need to double enter and no further action is required.
We have enabled a feature in askmyGP which allows you to specify a role, compatible with GPAD reporting, for each staff member. We suggest you state a suitable role from the drop down list in the staff record, which is done only once and would take a few minutes for the whole practice. Any reporting needs should then automatically be covered.
- Published in News
How askmyGP is providing a system that works for everyone at The Grove Medical Centre
Summary
Over the past year, many GP practices have turned to askmyGP to help them navigate the challenges the pandemic has presented. The Grove Medical Centre in Swansea, which covers a patient population of approximately 7,500 people, has been using askmyGP since April 2020. We spoke with Dr Jack Williams, one of the four GP partners at The Grove, about his experience of the system and the benefits it offers the practice.
Triage system working for all types of patients
Before the pandemic, the system in place at The Grove ensured patients always experienced excellent availability of appointments, with almost all patients being seen on the same day they requested an appointment. There was no triage system in place as there was no need for one. When Covid-19 began to surge in the UK, the practice team decided that a triage system would be vital to maintain the quality of service and for the safety of patients and staff. Following a short implementation period, The Grove launched askmyGP at the beginning of April.
The team wasn’t sure how patients would take to it, but the initial feedback they received was very positive. Dr Williams says: “What we found was that it was actually a very good time to implement a new system because the pandemic meant people were more accepting and understanding of the need to change.”
The Grove has a wide patient demographic, with many different ages and levels of deprivation represented. The practice has found that most people have been able to use the new system with no problems, with the data showing that even patients over 90 are accessing the practice online.
The practice expected a small number of people would still need to access the practice via phone, however, as Dr Williams explains: “We are encouraging people to go online, but that is not a barrier – we knew there would be people who don’t have access to the internet and these patients tend to be our more vulnerable members of society. The phone lines are still open, and in fact askmyGP has benefitted these vulnerable patients by making our phone lines less busy for them, so those that do call find it easier to get through.”
No effect on clinical judgement or prescribing activity
An area of concern around the increased use of digital tools such as total triage and remote consultations has been the effect this may have on clinical prescribing behaviour. Health Foundation research, however, found no significant evidence of the askmyGP model affecting prescribing rates. This aligns with the experience of GPs at The Grove Medical Centre.
Dr Williams says: “For us, it’s not all about e-consulting. Yes askmyGP allows us to e-consult, but the benefit for us is that it is a triage system with the capability to do an e-consult if we wish. We can respond to people with a message on the system, but we will still call the patient or conduct a patient examination if needed. We are conscious not to allow these new ways of consulting affect our clinical judgement and our data shows that we actually see more patients face to face, than are requesting this type of consultation.”
Matching demand and capacity to ensure requests are resolved quickly
The practice team was keen to ensure that they were able to continue resolving as many requests as possible on the same day they came in. The data askmyGP provides The Grove shows that requests are resolved on average 116 minutes after they were made. The data also enables a more proactive approach to staffing, as the practice is able to predict demand at weekly, daily, and even hourly levels.
This has been enormously helpful during the pandemic, says Dr Williams. “The visibility of demand that askmyGP offers has enabled us to rearrange rotas and match our capacity to that. This also helps with staff morale, as it means we can aim for all the staff being equally busy on different days.”
Image: Swansea Marina © Crown copyright (2013) Visit Wales
- Published in Case studies
How do access hours affect online GP demand?
Demand in general practice is high for the time of year, not just in the media but in the data. It may result from a combination of changes coming out of lockdown, delays in secondary care or easier access, but we don’t have convincing evidence of which is most significant.
The question of what to do about it can’t be separated from the cause, as a wrong diagnosis and resulting wrong solution may make the situation worse. Some have speculated that easier access online is driving up demand, which sounds logical although we saw no evidence of that pre-covid. Nevertheless, if better access has uncovered unmet need that was there all along, what should be done?
One suggestion is to reduce the hours in which online access is available, and Steve Black has taken a look at the outcomes in terms of total demand as a % of list size, since the start of 2021. In the first example, online is available 24/7, although patients are told if they are out of hours to expect a reply on the next working day. Grey bars represent availability, and the red line shows total demand.
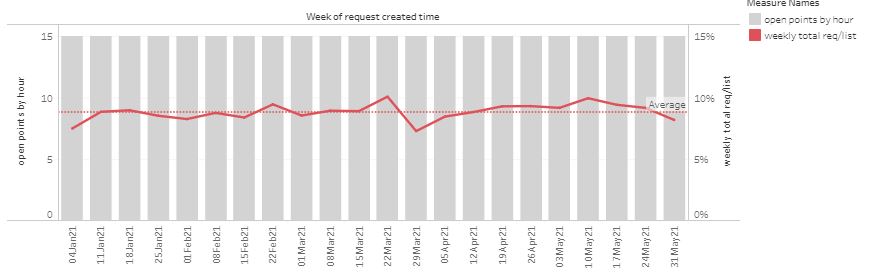
“Open point” is a score based on the period when patient requests can be submitted, weighted towards normal contracted hours. The red line is total demand (online and telephone requests) as a % of list size, per week.
In the following example, opening hours were cut in response to perceived high demand.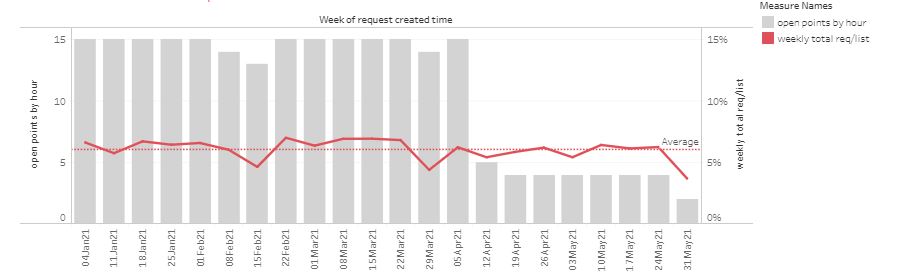
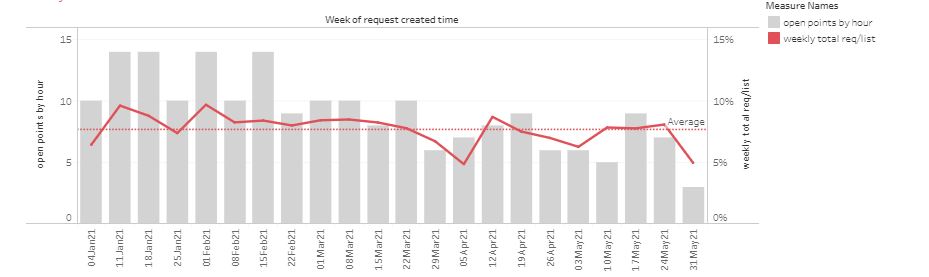
Another practice has made multiple changes in an attempt control demand, sometimes significantly reducing availability even in-hours.
 Overall, changing opening hours has had little effect on demand. However, as a patient there is a loss of service as they cannot be so sure they can submit a request online when they want to. Constantly changing the time the system is turned off risks patients losing trust in the online route, driving more demand through the telephone route which is less efficient to manage.
Overall, changing opening hours has had little effect on demand. However, as a patient there is a loss of service as they cannot be so sure they can submit a request online when they want to. Constantly changing the time the system is turned off risks patients losing trust in the online route, driving more demand through the telephone route which is less efficient to manage.
Taken to the limit, turning off online access completely would return to purely telephone access, with none of the flexibility for both patients and staff to use the efficiency of messaging and workflow.
Are there other advantages in cutting hours? Some take the view that they feel more in control if they know that no new requests can arrive after a certain time. Others turn off access at weekends, on the basis that some issues may have self limited by Monday, or they don’t want to see requests stored from the weekend, adding to a busy Monday.
Our usual advice to practices has been to keep online access open all the time, both in-hours and for OOH times when the message to patients sets a different expectation. However, we are clear that practices may turn off access themselves, either routinely or ad-hoc for example in the case of staff absence.
Based on the new data, we would suggest:
1. Reducing access hours has very little effect on total demand.
2. Practices may choose to limit hours, and it’s better to have consistent times so patients can be confident that online is open.
3. Whatever the decision, it should be up to the practice to determine access hours, and easily controlled by practice staff.
- Published in Evidence





