Personal or personalised?
I’ve been reflecting recently on what we mean by personal care. NHS England’s Head of Digital writes of the NHS Long Term Plan this week:
”… sets out an exciting ambition for care that is more personalised and tailored around the needs of the individual, enabling people to have more autonomy over their health and wellbeing. It describes a future where people will be empowered to participate in their care using digital services that truly meet their needs, help them live better with long term conditions, target prevention and offer them a much more personalised experience.”
No doubt the intention is good but I’m concerned that what we design and build should be grounded in the everyday needs of patients, and I don’t hear them using that language.
We get over 500 patient feedbacks each week and one of the strongest themes is thanks to a doctor or nurse they name.
What we hear from patients if I could summarise in a sentence is: “I need help with my medical problem from someone I trust.”
For patients, personal care faces outwards, they are dealing with another person they know and trust.
“Personalised” seems to me inward facing, a digital experience where the technology is configured with my preferences and perhaps my medical history. It might be clever and it might have value, but I’m not hearing from patients that they want autonomy, especially those who are most in need of help.
“Personal” brings us back to that question of continuity of care. It’s well documented to have fallen in recent years, but we also know that this is not inevitable.
Some I think seem to view continuity as a kind of spiritual nirvana, or a lost golden age where the family doctor had all the time in the world for everyone who dropped in to see them.
Back on earth, right now, it’s a simple operational problem of “Can a patient needing help choose a named clinician?”
We’ve always made this possible with a validated list shown to patients, of all clinicians working today, and around 20 – 30% of patients make a choice. But we’ve just introduced three improvements to make it easier both for patients and practices, since ease of use is the biggest driver of any change.
- While the patient may only choose someone working today, they can now look a week ahead to see when their chosen GP is available (they always have capacity same day)
- With our One Click Assign feature, a GP if named is starred so unless there’s a reason not to, the assigner will, with one click, put that patient request in front of said GP.
- Any patient can have a “Usual GP” set, if the practice wishes, so even if the patient doesn’t choose, the assigner can see that GP tagged with an icon in the One Click Assign list.
The outcome is that we are hearing every day from GPs and patients who feel empowered.
There’s a growing conversation on Twitter (follow @askmygp) from all sides, do take a look.
Dr Lis Flett writes “Accessibility, Continuity. Responsiveness. Compassion. From your own GP. That is what modern UK primary care needs.”
Some years ago I heard former RCS President Clare Marx speak and I have often quoted her words, “We must make the digital, personal”. So true, and yet I wonder whether she has been heeded?
Perhaps to make this work we should look at it the other way round.
“We need to enable the personal with digital”
That’s the task for NHS England’s Head of Personal.
Regards
Harry Longman
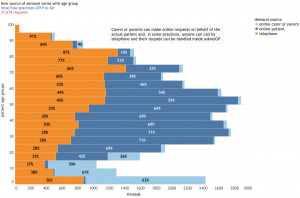
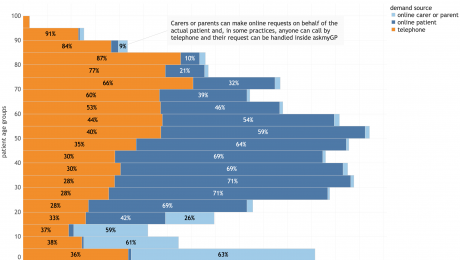
PS Data geeks, this is fascinating. We’ve just published a study showing the age-specific adoption of online consultations. Covering 10 practices in the period 1/1/19 to 8/2/19, n = 37,634 requests, it shows that for young adults 70% are now seeking help online rather than by telephone, and even up to 65 it’s over half. These are normal regular local digital first practices.
Chart and notes here: Age specific adoption of online consultations.
PPS 4 new practices and another 30,000 patients covered last week, with Weston-super-Mare reaching half way in its project for the whole town.
- Published in Comment
Age specific adoption of online consultations
Context
The latest data from our chief analyst Dr Steve Black (@sib313) shows remarkable adoption of online consultations across all ages and 10 diverse practices. n = 37,674 requests, date range is 1/1/2019 to 8/2/2019.
The context is all askmyGP practices operating in “total flow” mode where all patient demand goes through the system in two modes. Online, patients submit a request for help from their NHS GP practice either for themselves (dark blue) or as a proxy (light blue), mostly children but also vulnerable adults, most over 75. They may also telephone the practice, and a receptionist creates the request on their behalf (orange).
The key point is that all demand is covered in the chart, not from a self-selected subset of patients, and these are regular GP practices where there is no change in registration.
What the data shows
For infants and children, over 60% of parents chose to send their request online.
For young adults aged 20 – 40, over 70% submitted online.
With increasing age, the proportion online falls slowly, but even at 65 – 70 it is 40%.
Over 70 the proportion falls more steeply and significant numbers are by proxy.
Policy implications
It is clear that when designed for ease of use and universality in respect of patients and their medical problems, coupled with rapid response by providers, the online offer is highly attractive to patients.
The vision for “digital-first” providers who are at the same time traditional, local GP practices is achievable and already being achieved.
Harry Longman
Founder, Chief Executive, askmyGP
- Published in Evidence
The network’s the thing
I’ve had a bit of time to absorb the new GP contract – there’s an excellent summary on GP Online if you don’t want to read it all. While some of the digital notes are a tad off key, I suspect they are a nod to our technophile SoS while the real action is elsewhere.
The centrepiece is Primary Care Networks, PCNs, and we are going to hear lots and lots more about them. Notice how the language has changed, as until quite recently it was all about “GP at scale”, a phrase absent from both BMA and NHS England texts.
Hats off to Richard Vautrey and team.
While the numbers “30 – 50,000” are the same, rather than large scale providers for which no convincing evidence was ever produced, networks of existing providers with no change of scale could make sense.
Steel mills need economies of scale, but GPs don’t, and diseconomies of scale soon show up with loss of continuity, local accessibility and lower patient satisfaction all well known.
But some AHP resources don’t really work at smaller practice level, and it’s clunky to employ for example a pharmacist for 7 hours a week and a physio for 12. At the network level they could work well, and indeed this could rebalance the funding model in favour of smaller practices as funds and resources will be based on list size.
The DES incentivises all practices join a network, and there will be a dash to join up with “people we like” at the local level. Expect a few funny shaped contiguous groups, some larger and some smaller than prescribed, but with a little pushing and shoving the money will ensure it happens.
The labels don’t all say this, but a very large proportion of the new money will effectively go into core funding, and will strengthen GMS partnerships as indeed the Watson review said they should be strengthened. This is a good thing for GP, for the NHS and the population as a whole.
The new and interesting questions arise over how the networks will operate. 22,000 new primary care staff is a lot to take on board, considering only how they are recruited, trained and managed.
Any shared resource raises the problem of “the freedom of the commons”. Currently, the design of A&E, urgent care centres, 111 and so on means they soak up demand from poorly performing GP practices. The reward for failure is for someone else to take your work.
How will the the new AHPs be shared fairly, so quality is rewarded as it should be? (by the way, fair is not the same as equal. Consider the student practice in the seaside town)
Practically, how will GPs make best use of them, appropriately referring the right patients at the right time? What is the patient view?
How will network performance be measured? How soon will patients get the right help? How will outcomes show we’re getting value for money?
No doubt we will return to these themes.
Cogitate as well as celebrate this weekend.
Harry Longman
PS No network yet, but already there with 100% of patients offered online and video consultations, Dr Barry Sullman talks about Balaam St Surgery and astonishing return on investment.
He’s a traditional, local, digital-first practice. Fabulous.
- Published in Comment
New GP contract: more work, less output
Hurrah! NHS England and the BMA GPC have agreed a new contract covering the next five years.
Apparently there’s lots more money, funding for 22,000 addtional health workers in primary and community care, and everyone seems very happy with it. I couldn’t possibly digest the whole lot but will concentrate on what we know best.
This is going to increase GP workload and cut patient access.
How so? See the fine print in the IT and digital section.
1. NHS111 will have the right to book directly into 1 appointment slot per 3,000 patients (rounded down) per day.
Leave aside the technical issues, problems of policing the scheme and arguments over unused slots, late booking and so on, what would happen even if it did work perfectly?
In a traditional practice with more patient demand than available slots, they tend to be all booked up within minutes of reception opening. You know, we know, everybody knows.
So now what does the savvy patient do? Call NHS111. Go through all the palaver of identifying themselves, answering dozens of irrelevant yet scary questions, eventually landing with “I need to see the GP. And I have a right to one of those 2 appointments in my practice of 8,999 patients, today.”
Boom, they got it. But they got the second one and there is no way of telling the other 23 patients who were turned away by the practice, so all of them go through the NHS111 palaver again, but get the same message: all slots gone.
So we’ve wasted NHS and patients’ time, added a bunch of complexity, and increased GP capacity by precisely zero.
And by the way, what do GPs think of the ability of NHS111 to triage a patient and provide concise and relevant detail of the conversation? Do ask one.
2. Make 25% of appts bookable online?
It is now such a commonplace that we kind of assume everyone knows this: only about one third of patients seeking help from their GP need a face to face appointment.
Which means that if GP capacity is reserved for patients to decide for themselves to take a slot, two thirds will be wasted. So that’s 17% of GP capacity to be wasted by design. Maybe they will include telephone appointments, which would be less wasteful but still may not be appropriate.
Reserving any proportion for a single channel reduces equity of access: those with no online capability, often the most vulnerable and needy, are shut out of 25% of available capacity.
It could be so much better, simpler and cheaper.
Here’s what our practices are already doing:
1. When they are open, there is always capacity, so no need to call 111 to try for reserved slots. They won’t be used, but neither will the GPs waste the time, they’ll just crack on.
2. Make 100% of capacity available online – that’s normal, it’s what we do. But 100% of capacity is also available for patients who phone in – there is complete equity of access.
It’s the same capacity. But how it is used for each patient is up to the GP to decide, which they do in seconds through digital triage – they don’t even need to phone many patients.
It takes two to tango, and the tragic missed opportunity here is that both GPC and NHS are stuck in supply thinking: it’s all about pushing services at patients, wrapped up in complex funding rules.
Demand led thinking does exactly the reverse, understanding in great depth and detail the incoming demands and designing services around them. We’d get bucketloads of efficiency as well as astonishing performance if they did that. (Do call, best rates for hard up government departments)
Well, I always say that when they’ve tried everything else that doesn’t work, they’ll be back. Maybe before I’m dead.
Why take the risk, start now!
Harry Longman
01509 816293 / 07939 148618
PS We’ve been amazed by the views on our new video, Dr Barry Sullman talking about Balaam St Surgery.
He’s a traditional, local, digital-first practice. Fabulous.
- Published in Comment
They can’t both be right
Do you ever wonder about that phrase “local needs”?
It made me wonder whether say Facebook had ever been asked to do a local needs version.
It’s just that we are responding to tenders issued by different CCGs, which are remarkably different given that I thought patients had roughly the same range of diseases wherever they live.
Essential requirement A: “Is able to fully triage the patient and signpost to the most appropriate service with no GP intervention”
Essential requirement B: “The system should not perform an automated triage that gives a disposition”
Imagine a pharma procurement where A specifies that it shall raise the patient’s blood pressure, and B that it shall lower it.
There’s a national specification for online consultations and question of what the computer actually does with the patient request seems central to the whole scheme… you couldn’t make it up.
Whether it’s more surprising or saddening I don’t know, but there is now a subastantial body of evidence of what doesn’t work in online consultations, and it includes much of what is being specified:
– no safe & economic automated triage has been invented
– lengthy questionnaires lead to very low usage, under 1%
– there is no evidence of online channels reducing oveall demand.
Despite all this, specifications are full of wishful thinking which will simply result in more taxpayers’ money being flushed down the toilet.
But perhaps what’s less well known is the evidence of what does work.
We’re just about to release a new video case study which is an inspiration. Final checks are being done, and I’ll tell you all about it tomorrow.
Harry Longman
PS the GP in question wrote to me yesterday “I am laughing and dancing” When you see the video you might assume we paid them for it. No, they pay us from their own partner income, just a regular customer.
- Published in Comment
The NHS App and the toenail test
Today I return to that long term plan and a piece of it which has so tickled the national consciousness that it made the News Quiz.
To touch quickly on “Skype consultations”. Skype for various reasons is problematic – it requires both parties to have a login, whereas our video solution works with a one time link. But headlines have been overblown. We now know that when offered the choice, only about 1 in 1000 patients are choosing video. It may grow a bit, but I don’t see it becoming a huge channel.
Let’s move on to the NHS App.
I will share a little of my medical history, and I hope you don’t find this too much information, but I get fungal nail infection.
So in the interests of science I wanted to test how the NHS App would help with my condition, using its 111 online algorithm, and my presenting symptoms of “brown and broken toenails”.
You can see the whole process in this 3 minute video which is how long it took.
It asked me 12 questions, of which 1 was possibly relevant, 10 irrelevant and 1 frankly embarrassing. The outcome was self care, but with absolutely no specific advice on what to do.
I have tried the same input with the Babylon AI chatbot, which couldn’t find anything relevant and asked whether I had any more symptoms (as if the waiter told me the fish option was off).
I have tried the same input with EMIS Patient.info. Its first option was “Fibre and Fibre Supplements” on which I clicked, and they tried to sell me a hearing aid.
I have tried the same input with NHS Choices, and the first option was sepsis, that well known affliction of toenails, though it did have Nail Problems as the fifth item, which does have relevant information on fungal nail.
I gather about 10% of the population has this, and whenever I mention “brown and broken toenails” to a doctor, the first thing they say to me, without even looking, is “fungal nail”.
If the might of government, of major corporations and £millions of venture capital can’t get toenails right, what hope have they when conditions are complicated and serious? I must leave the question with those qualified to assess them.
On Twitter Dr Dave Triska writes:
“I consulted with 3 people today with a near identical ‘cough’ presentation, recognised the ill one (whom I knew to be stoic and was concerned they had contacted me). Guess what? Sick. As. Algorithm would have missed that.
I just tried my sick patient will all big 3 symptoms checkers. All falsely reassured. From an algorithm point of view, they were right. Likely URTI. Except it wasn’t…
How would I program into an algorithm that the barn door URTI I did also bring down needed to be seen because I knew they’d lost someone to lung cancer and would be worried? That a visit and chat helped them in ways that aren’t measurable against outcomes?”
All falsely reassured.
No doubt you find that very concerning, but consider the specification on which we were invited to bid by a CCG yesterday:
Essential criterion: “Is able to fully triage the patient and signpost to the most appropriate service with no GP intervention using a solution where indemnity lies with the supplier and not the practice”
You’re welcome.
Harry Longman
PS. We do offer self care help with askmyGP, but we don’t claim that it reduces demand or diverts patients. We aim to make it as fast and simple as possible. Please try it yourself, with “brown and broken toenails” or anything else. This is exactly what your patients would see.
Try Bramley Demo Surgery, patient facing
Did we meet the aim?
- Published in Comment
Encouraging, Dangerous, Lackadaisical
So the NHS long term plan has landed and it’s a techie one. Should we be happy?
As a part-time nerd myself I can’t help but feel the enthusiasm with the word “digital” appearing no less than 14 times in this single page on primary and outpatient care.
“Over the next five years every patient in England will have a new right to choose this (digital first) option – usually from their own practice or, if they prefer, from one of the new digital GP providers.”
I’m going to describe it with three words you wouldn’t normally put together.
Encouraging – Matt Hancock has clearly recognised how far behind the NHS is in patient service, and how new technology can help. I agree on tech enabled, but tech driven is something else.
Dangerous – shifting the ground rules to move patients away from their own local NHS GP will do immeasurable damage to the long term continuity of care integral to the registered list system, and in so doing undermine the professional careers of GPs. Test this idea against Prof Chris Salisbury’s Mackenzie Lecture – the transcript now with illustrations is a must read.
Lackadaisical – with many patients forced to wait three weeks for an appointment, why make them wait five years for change? We’re turning regular NHS practices into digital first practices overnight (well, with four weeks preparation, then overnight). Digital first because all patients are welcome online, but not forced online, and we’re seeing over 60% from day one.
Day one feedback, today: “Seeing its a new introduction, I think its fantastic. The helpfulness, the speed, and the results. Thank you.” Gentleman, 71, Weston-super-Mare.
Come on Matt, keep up!
Harry Longman
- Published in Comment







Taming the threat of digital first
Dear colleague,
“Private providers could grab unlimited share of GP consultations online” runs the heading in GP Online.
“Babylon GP at Hand given green light to expand NHS services into Birmingham” – to the usual outcry from BMA.
“All patients to have the right to video and online consultations by April 2020”. Have I got the right April? Why is it always April?
Let’s look at what GP at Hand have actually done in their 18 months of operation. At a cost of blanket advertising around the capital, they have recruited just 40,000 or one in 200 Londoners to their video-led service. I hardly think this merits the cries of barbarians at the gates.
But as we know people are led by feelings much more than facts, and all the headlines are designed to scare you.
They want you to feel threatened, that your livelihood is at stake.
They want it to “feel like” extra work – because anything ordered by the government must be extra work.
They want you to “feel like” you are being bullied into change, you’ll have to be different, and you don’t want it to be different, you didn’t sign up for this, and what do they know about your real work?
It’s a shame because very few GPs have considered the possibility that with the right design, digital first could enable you to be a better GP, providing a better service for patients with less work.
A practice we’ve worked with for eight months now is Witley and Milford, and some of their GPs were discussing the outcomes on Twitter this week. They are one of our fastest operators, with a median time to complete patient requests of 48 minutes (that’s all demand acute/routine whatever, and that’s completed, not just first response). They are also one of our highest for continuity, with 94% of patients who made a choice being helped by their chosen clinician.
All they have done is understood demand and flow and organised themselves around those principles. With over half their demand arriving online, they are a digital first practice, and it’s a joy to be a GP or a patient.
Many sage commentators tell us of the trade off that must inevitably be struck between Access and Continuity. I tell them Witley and Milford.
Best regards,
Regards
Harry Longman