How askmyGP is providing a system that works for everyone at The Grove Medical Centre
Summary
Over the past year, many GP practices have turned to askmyGP to help them navigate the challenges the pandemic has presented. The Grove Medical Centre in Swansea, which covers a patient population of approximately 7,500 people, has been using askmyGP since April 2020. We spoke with Dr Jack Williams, one of the four GP partners at The Grove, about his experience of the system and the benefits it offers the practice.
Triage system working for all types of patients
Before the pandemic, the system in place at The Grove ensured patients always experienced excellent availability of appointments, with almost all patients being seen on the same day they requested an appointment. There was no triage system in place as there was no need for one. When Covid-19 began to surge in the UK, the practice team decided that a triage system would be vital to maintain the quality of service and for the safety of patients and staff. Following a short implementation period, The Grove launched askmyGP at the beginning of April.
The team wasn’t sure how patients would take to it, but the initial feedback they received was very positive. Dr Williams says: “What we found was that it was actually a very good time to implement a new system because the pandemic meant people were more accepting and understanding of the need to change.”
The Grove has a wide patient demographic, with many different ages and levels of deprivation represented. The practice has found that most people have been able to use the new system with no problems, with the data showing that even patients over 90 are accessing the practice online.
The practice expected a small number of people would still need to access the practice via phone, however, as Dr Williams explains: “We are encouraging people to go online, but that is not a barrier – we knew there would be people who don’t have access to the internet and these patients tend to be our more vulnerable members of society. The phone lines are still open, and in fact askmyGP has benefitted these vulnerable patients by making our phone lines less busy for them, so those that do call find it easier to get through.”
No effect on clinical judgement or prescribing activity
An area of concern around the increased use of digital tools such as total triage and remote consultations has been the effect this may have on clinical prescribing behaviour. Health Foundation research, however, found no significant evidence of the askmyGP model affecting prescribing rates. This aligns with the experience of GPs at The Grove Medical Centre.
Dr Williams says: “For us, it’s not all about e-consulting. Yes askmyGP allows us to e-consult, but the benefit for us is that it is a triage system with the capability to do an e-consult if we wish. We can respond to people with a message on the system, but we will still call the patient or conduct a patient examination if needed. We are conscious not to allow these new ways of consulting affect our clinical judgement and our data shows that we actually see more patients face to face, than are requesting this type of consultation.”
Matching demand and capacity to ensure requests are resolved quickly
The practice team was keen to ensure that they were able to continue resolving as many requests as possible on the same day they came in. The data askmyGP provides The Grove shows that requests are resolved on average 116 minutes after they were made. The data also enables a more proactive approach to staffing, as the practice is able to predict demand at weekly, daily, and even hourly levels.
This has been enormously helpful during the pandemic, says Dr Williams. “The visibility of demand that askmyGP offers has enabled us to rearrange rotas and match our capacity to that. This also helps with staff morale, as it means we can aim for all the staff being equally busy on different days.”
Image: Swansea Marina © Crown copyright (2013) Visit Wales
- Published in Case studies
General Practice Appointment Data – reporting to NHS England
In order to help you meet your GPAD obligations, and improve reporting in the practice, staff ‘profession’ needs to be recorded consistently. This note explains the process, context and wider benefits.
English Practices have recently been asked to provide appointment data via their CCGs to NHS England. As you will know, we believe that a flexible triaged approach supports practices to utilise their time to best effect for themselves and their patients. This view appears to be reflected in NHS England’s guidance on ‘total triage’.
We remain in discussion with NHS England, because we feel that you are being asked to report data that may not accurately reflect the activities carried out in the practice. In addition, we have made some changes to resolve the immediate issue, which is to minimise the administrative burden for you in completing the reports.
To enable a report to be produced, consistent descriptions of ‘profession’ are needed to meet the GPAD requirements. Pragmatically, this means that all staff professions need to match one of the exact descriptions recognised by NHS England. The new ‘Professional Group’ list allows you to select the best match for each staff member. This is accessed via Staff > Edit, or Settings > My Profile. There is a short note available: https://askmygp.zendesk.com/hc/en-gb/articles/360006981297
Although this work is in response to GPAD, there are some more general benefits. By using consistent descriptions of profession, we will be able to provide you with better reporting in relation to staff groups – for instance allowing capacity planning by profession, or better understanding the activity of groups within the practice.
As always, the quality of any reports produced are dependent on the quality of the input data. Obvious limitations of reports from askmyGP, besides data quality include:
- any activity not recorded via askmyGP will not be included e.g. Nursing or Clinic activity booked directly.
- We cannot report on data (such as profession) which has not been entered into the system.
- GPAD guidance permits some contacts to be counted twice. We will try to ensure that we include this, however it may not capture a small percentage of this double activity contact.
We will add a report to your system in the near future. Should you wish us to provide reports directly to your CCG please contact us via your Training Partner to discuss details.
- Published in News
Patient preferences and clinicians’ choices in 2020
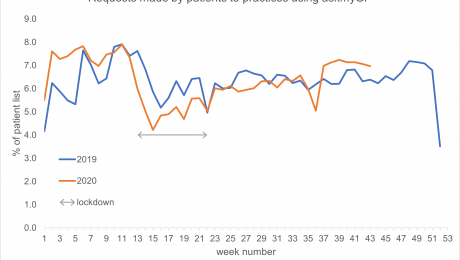
Perhaps surprisingly, latest figures from askmyGP showing patient contact activity are consistent with those from the equivalent period in 2019. Data show similar volumes of demand by patients, at approximately 6% of the practice list size making a request per week.
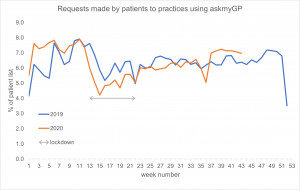
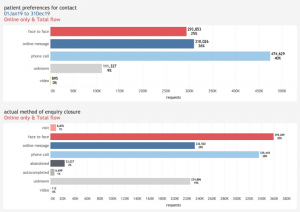
When offered a choice of ways to talk to their GP, 12% of patients expressed a preference for a face-to-face appointment, 34% preferred to be contacted by secure message and 50% by phone. Despite the obvious changes in methods of communication clinicians have continue to deliver care to their patients at a similar rate despite the effects of Covid.
Comparisons between years
Overall volumes of activity, expressed as percentage of the practice list making a request of their GP practice, are very similar when the same week is compared between 2020 and 2019. For example, the effects of the Christmas and Easter breaks can be observed in both years (Easter was slightly earlier in 2020), alongside e.g. public holidays in early and late May. Activity throughout the summer is nearly identical between years.
Communication methods
While similar proportions of cases were resolved, the mechanisms used to do so have changed substantially between years. Compared to 2019, responses to patients made less use of face-to-face and more use of secure messages and telephone consultation – the effects of Covid precautions being the most obvious explanation. Visits dropped from 0.92% to 0.53% and video usage remained low at 0.33% (not shown).
The askmyGP data is drawn from practices with diverse patient populations receiving a total of 4,067,068 patient requests during the year to date. The data illustrates patient contact by clinical episode, with video consultation and secure messaging with the patient’s usual NHS GP offered at no extra cost to either the practice or the patient.
Clinical judgement always takes precedence, meaning in some cases simple queries might be addressed by a quick answer by phone or message, while more complex presentations will warrant a face-to-face appointment, even in cases where this has not been requested by the patient. Practices are not bound by their patients’ contact preferences, but they use the information to guide their responses to patients.
Recent analysis by The Health Foundation similarly found that consultation rates changed only slightly – at askmyGP practices activity decreased by less than 1% between 1 March–30 June 2020, compared to the same period in 2019. However, they found there has been a dramatic swing away from face-to-face consultations. Between 1 March–30 June 2020, 8.5% of appointments were held face-to-face, compared to 38% during the same period in 2019. Use of remote consultation methods increased. Telephone appointments increased from 39% to 51%, online message from 23% to 40% and although video increased 50-fold, it remained low at 0.5%.
3 November 2020
- Published in Evidence
Celebrating five million patient requests
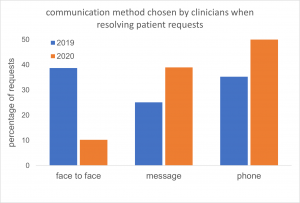
Five million patient milestone reached by online consultation and workflow system askmyGP
Five million patient requests have been managed by GP practices using the askmyGP online consultation and workflow system since September 2018. The system is used by practices throughout the UK with a combined list size of over 2 million patients. Clinicians at the practices use the system’s online triage tools to prioritise and deliver care by secure message, telephone, video or face-to-face appointment.
In those requests, 70% of patients chose to contact their GP online via the practice website, while the remaining patients phoned their practice. Half of patient requests were completed by the practice in two hours or less, including requests made online outside normal surgery hours.
Overall, patients asked for face-to-face appointments in only 12% of cases. 50% of patients asked to be contacted by the practice by phone and 34% asked for a secure message from their clinician. This pattern has varied considerably due to lockdown, with a clear shift away from face-to-face activities.
Across those patient requests, clinicians decided to see 12% of patients face-to-face. 86% of patients’ requests were resolved on the same day they contacted the practice. Recent patterns differ somewhat and can be explored in the live data presented on our website.
Across the five million patient requests, between 5% and 7.5% of patients on the practice list made contact each week; we observed that seasonal fluctuation is greater than the changes observed during lockdown. Patterns of demand in 2020 have remained similar to 2019 – this point is discussed further in our blog: patient preferences and clinicians’ choices in 2020
The five millionth patient request was received by the St John’s Medical Centre in Altrincham, early one Thursday in October 2020. St John’s has been using askmyGP to manage all of its patient requests since January this year. The request was closed by telephone 51 minutes later. GP partner Dr Marik Sangha said:
“With askmyGP we are simply getting through the work more efficiently. Although we are supporting the same numbers of patients, most don’t need to come into the surgery – you don’t need to physically see them. Nearly 80% of our patients make their request online, freeing up phone capacity for our more vulnerable patients who need more help. Patient feedback has been extremely positive.”
Harry Longman, chief executive of Salvie Ltd, the company behind askmyGP, said:
“This is a major milestone, and we are delighted that askmyGP continues to enable patients to get help promptly from their own GP. Despite the challenges presented by the Covid pandemic practices are able to understand, predict and manage patient demand much more flexibly, putting them in control of who they see and when, and ensuring patients receive appropriate support despite challenging circumstances.”
3 November 2020
- Published in Evidence
Weston askmyGP Case Study
In September 2018 a year-long project was initiated by the local CCG to support recruitment and retention in Weston-super-Mare, which has the highest proportion of GPs and nurses in the CCG area nearing retirement.
With significant demographic pressures from a population that is both ageing and growing, practices in the town and surrounding villages were under severe pressure with an unsustainable workload. Many practices were relying on locum doctors to fill sessions.
With askmyGP fully implemented at New Court Surgery life for the practice team has been transformed. Patients contact the practice by phone or via the practice website, with all requests processed through askmyGP. Doctors review all requests and allocate them to the most appropriate team member to deal with.
Dr Heather says: “There has been a massive improvement in the flow of patients through the surgery and patient satisfaction is generally very high. The clinicians are more in control and we are able to deliver good access alongside great care.
Read more in the case study: NewCourt
- Published in Case studies
Contact Patient preferences and clinicians’ choices in 2019
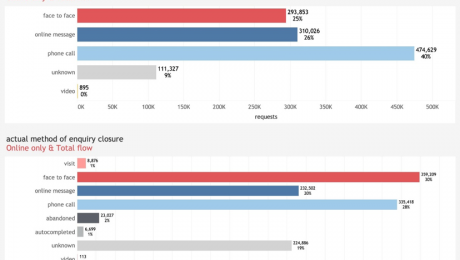
The 2019 full year figures from askmyGP reporting patient contact preferences show that when offered a choice of ways to engage with their GP Practice, 25% of patients expressed a preference for a face-to-face appointment, 26% asked to be contacted by secure message and 40% by phone. Data show continued low demand among both patients and clinicians for video consultations (0.08%).
Clinical judgement always takes precedence, meaning in some cases simple queries might be addressed by a quick answer by phone or message, while more complex presentations will warrant a face-to-face appointment, even in cases where this has not been requested by the patient. Practices are not bound by their patients’ contact preferences, but they use the information to guide their responses to patients.
The flow diagram illustrates the transitions between these ‘requested’ and ‘actual’ methods of delivery, indicating that the greatest shift was for patients who had asked for a phone call, but clinicians decided that a face-to-face appointment was needed. The result of these transitions was that clinicians resolved 30% of enquiries face-to-face, 20% via message and 28% by phone. In each case, clinicians were able to make use of the clinical presentation and medical history when selecting how best to address the patient’s needs.
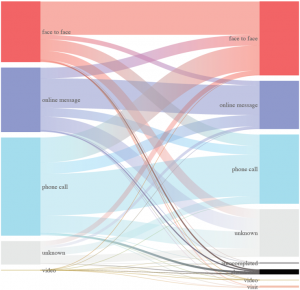
The askmyGP data is drawn from practices with diverse patient populations receiving a total of 1.2 million patient requests during the period. The data illustrates patient contact by clinical episode, with video consultation with the patient’s usual NHS GP offered at no extra cost to either the practice or the patient. Unknown refers to cases where the preference was not recorded, even though help was provided to the patient.
25 February 2020
- Published in Evidence
Celebrating one million patient requests
One million patient milestone reached by online consultation and workflow system askmyGP
One million patient requests have been managed by GP practices using the askmyGP online consultation and workflow system since September 2018. The system is used by practices across the UK with a combined list size of 545,485. Clinicians at the practices use the system’s online triage tools to prioritise and deliver care by secure message, telephone, video or face-to-face appointment.
64% of patients chose to contact their GP online via the practice website, while the remaining patients phoned their practice. Half of patient requests were completed by the practice in two hours or less, including requests made online outside normal surgery hours.
Patients asked for face-to-face appointments in only 25% of cases. 45% of patients asked to be contacted by the practice by phone and 30% asked for a secure message from their clinician.
On reviewing patient requests, clinicians decided to see 37% of patients face-to-face. 88% of patients who needed an appointment attended the practice on the day they contacted the practice.
Across the one million patient requests, 6.5% of patients on the practice list made contact each week.
The one millionth patient request was received by the Concord Medical Centre in Bristol, which has been using askmyGP to manage all of its patient requests for more than two years. Senior partner Dr Simon Bradley said: “With askmyGP we are getting through the work more efficiently and continuity of care has improved too, with more patients consulting with their preferred GP. There are days where all outstanding consultations have been completed by 5.30pm, allowing the duty GP to manage urgent problems and process late requests that otherwise would have been passed forward to the following day.”
Harry Longman, chief executive of GP Access Ltd, the company behind askmyGP, said: “This is a major milestone and we are delighted that askmyGP has enabled a million patients to get help sooner from their own GP. That’s only possible by making it easier for practices to understand, predict and manage patient demand much more flexibly, putting them in control of who they see and when, managing their resources appropriately for each patient.”
- Published in Evidence
Patient preferences and clinicians’ choices in Q3 2019
The latest figures from askmyGP reporting patient contact preferences are consistent with those from earlier in the year. Data show continued low demand among patients for video consultations (0.06%).
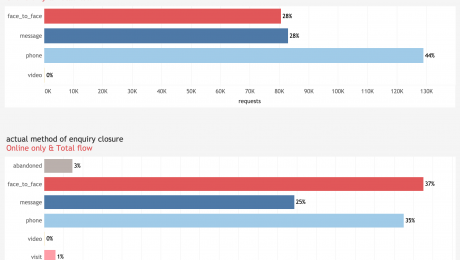
When offered a choice of ways to talk to their GP, 27% of patients expressed a preference for a face-to-face appointment, 28% preferred to be contacted by secure message and 44% by phone. Slightly more patients asked for a face-to-face appointment than in previous months, but clinical decisions and actual method of delivery remain consistent.
The askmyGP data is drawn from practices with diverse patient populations receiving a total of 308,000 patient requests during the period. The data illustrates patient contact by clinical episode, with video consultation with the patient’s usual NHS GP offered at no extra cost to either the practice or the patient.
Clinical judgement always takes precedence, meaning in some cases simple queries might be addressed by a quick answer by phone or message, while more complex presentations will warrant a face-to-face appointment, even in cases where this has not been requested by the patient. Practices are not bound by their patients’ contact preferences, but they use the information to guide their responses to patients.
13 November 2019
- Published in Evidence
Latest figures continue to show low demand for GP video consultations
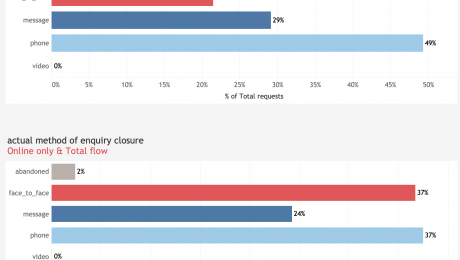
The latest figures from askmyGP reporting patient contact preferences show there has been no change in the low demand among patients for video consultations.
The askmyGP data for the second quarter of 2019 is drawn from practices with diverse patient populations receiving a total of 220,000 patient requests during the period. The data illustrates patient contact by clinical episode, with video consultation with the patient’s usual NHS GP offered at no extra cost to either the practice or the patient.
When offered a choice of ways to talk to their GP, 21% (Q1 25%) of patients expressed a preference for a face-to-face appointment, 29% (Q1 28%) preferred to be contacted by secure message and 49% (Q1 47%) by phone. Patients requested a video consultation in less than 0.1% (Q1 0.1%) of cases.
While practices are not bound by their patients’ contact preferences, they use the information to guide their responses to patients. Clinical judgement always takes precedence, meaning in some cases simple queries might be addressed by a quick answer by phone or message, while more complex presentations will warrant a face-to-face appointment, even in cases where this has not been requested by the patient.
13 August 2019
- Published in Evidence