How an online total triage solution improved patient experience and is helping to increase capacity – Jonathan Kerry, Associate Director of Primary Care explains
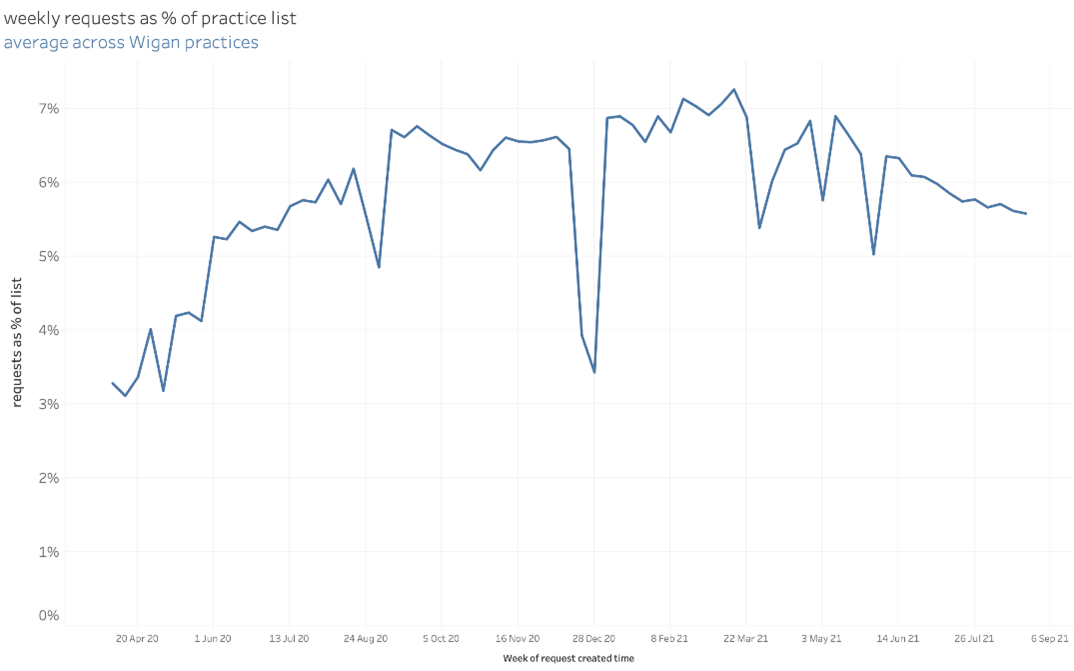
NHS Wigan Borough CCG has 58 GP practices varying in size from small to large. One of its larger practices has a patient list of 17,500 patients, while the average is around 5,000. Until the COVID-19 pandemic hit, just a handful had made the switch to digital working and total triage solutions. However in March 2020, when the doors shut, most practices faced a rapid implementation of digital systems to ensure GPs could continue to provide a service to their patients. The CCG recommended the askmyGP total triage solution and throughout the primary care networks (PCNs) practices started working together to learn from and support one another. Since then, the practices of Wigan have managed over one million patient requests via the askmyGP system, providing an extensive and robust dataset with which to improve ways of working. As well as improving the patient experience, data from askmyGP provides actionable insight, highlighting ways in which workflows can be improved by creating capacity and ensuring all patients are seen by the right person at the right time, while also helping to relieve the significant pressures currently being felt by GPs.
Standardisation leads to greater collaboration and new ways of working
When the COVID-19 pandemic took hold, the shift to digital had already been specified by the CCG within its primary care contracts. Many practices were behind schedule, but consideration also had to be given to how a total triage system could take healthcare forward. The CCG wanted to look beyond the pandemic to improving capacity and access in the future rather than just being a bolt on option giving patients an additional way to book an appointment.
Jonathan Kerry is Associate Director of Primary Care for NHS Wigan CCG. He says the PCNs supported this approach while also encouraging as much standardisation as possible across the system. He says: “If you can standardise at PCN level it makes it easier for practices during a challenging time. Even if it’s just sharing staff and providing resilience these are still worthwhile benefits.”
The push for standardisation was successful. Currently there are 43 practices out of 58 using askmyGP, giving 24/7 access to GP services. Jonathan says: “It helps to identify who is in most need, those who might need face to face or a different type of consultation method.
The PCNs supported standardisation between practices by creating working group forums, aiding learning about how askmyGP can be used to increase efficiency and make positive change. Having already worked together in the form of neighbourhood clusters since 2013, there were ready-made working groups for many clinical leads such as practice managers and nurses as well as patient forums.
Bringing everyone together to discuss any challenges or concerns meant that it was possible to take insight from askmyGP and create an action plan for change. Key to the success of the system is being able to offer core GP services and 24/7 access, but also helping patients to understand if other services can provide the help they need.
A recent snapshot survey by Pulse has revealed that waiting times for GP services across the UK came down during the pandemic as a result of online triaging and remote consultation.
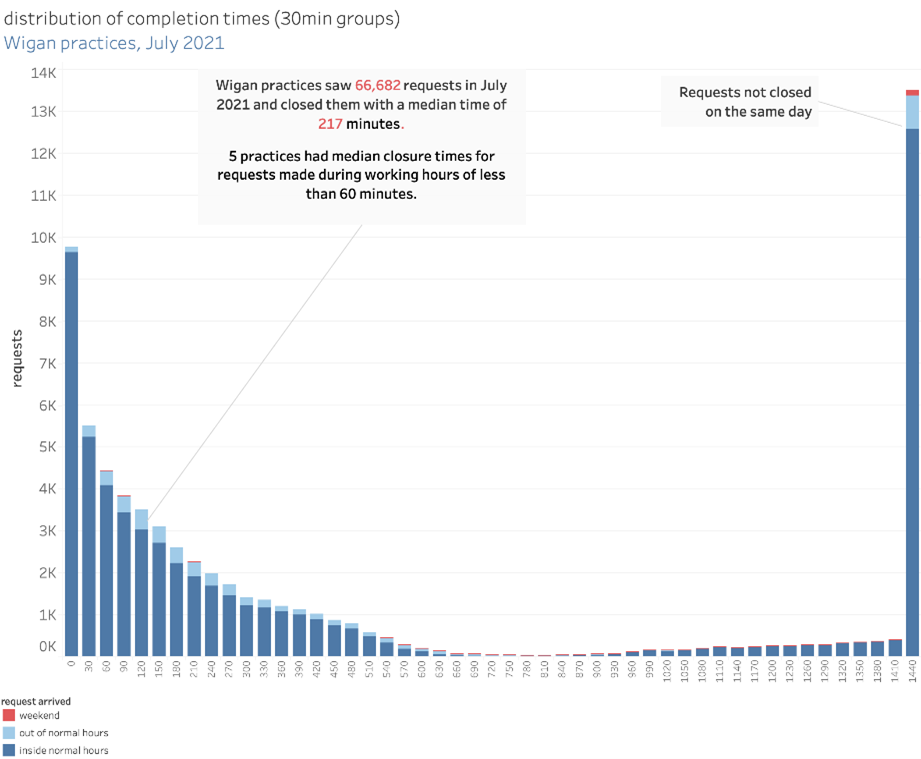
The findings from May reveal the average waiting time for a non-urgent in-person appointment following triage is down to 8.7 days, while the average wait for a phone or video consultation is 7.4 days. GP practices in Wigan using askmyGP have achieved a median waiting time of just 217 minutes.
However demand has risen, and GPs are doing more consultations than ever, creating significant pressures. By having several surgeries operating from the same system, it can mean sharing responsibilities rather than having all those surgeries simply replicating the way they work.
For example the PCNs in Wigan CCG have collaborated with a First Contact Physio initiative, which aids triage, helping to signpost the patient to the most appropriate person, rather than automatically seeing the GP as the first port of call.
Jonathan says: “It may not be a physio, but a social prescriber or community link worker. We just need to be able to get patients to the person who can help them and support them best. We can use the technology to underpin that and support them.”
“This is a good example of how to start, it was a rapid implementation to help practices during the COVID-19 pandemic, but the way that we are using First Contact Physios shows the potential and longevity of that way of working.
Expanding capacity and creating new ways of working
The introduction of online triage has been a broadly positive move for patients.
Feedback from the Friends and Family Test has been significantly higher than it has ever been. Over the last 12 months ratings have ranged from 75 to 90 per cent of people saying the service has been better or excellent compared to previous visits. “From a patient point of view, generally there is real positivity for it,” says Jonathan.
There are also encouraging signs from the National GP Patient Survey, taken in the first three months of 2021, which has shown the CCG area to be higher than average in its use of digital and around access to GPs.
However, Jonathan acknowledges that, while online triaging can be extremely positive for many, there is the potential that it can exacerbate inequalities. He says: “This is something that is always going to be there, so we have to keep working at it and making sure we are doing the right thing.”
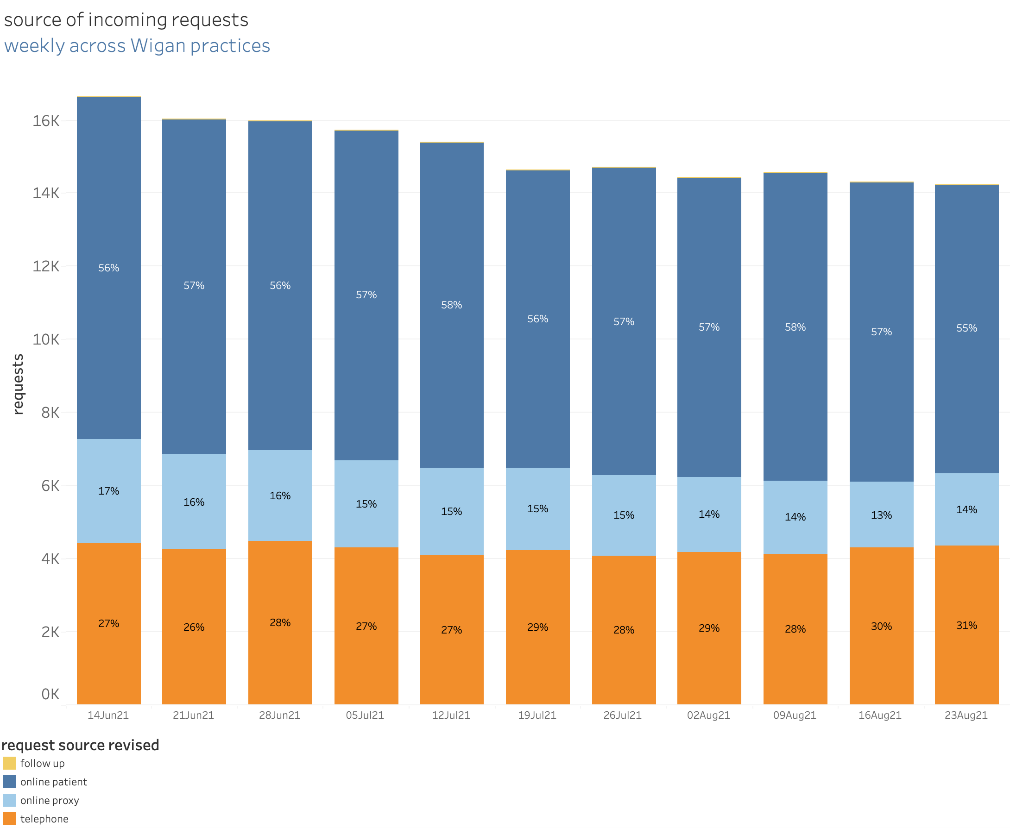
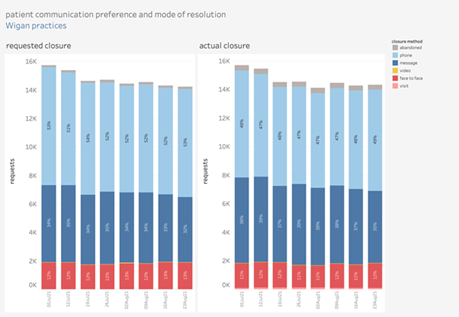
With askmyGP, patients can choose their method of contact. If they’re not online, the system is set up to ensure they get the same service should they need to phone the surgery or go in person. No-one should ever be forced to use the online system if they don’t want to.
The CCG is currently carrying out market research looking in more detail at the expectations of patients. Speaking to around 3,000 people, the CCG will formulate patient models to help them better understand patient need and see how they can evolve over the next decade.
Regular data can help surgeries hold a mirror up to the way they work
askmyGP generates data daily that can help practices track how they are working and focus on where change needs to be made. The data shows how the system is being used and the mechanisms which patients choose to make contact along with the reasons why.
Jonathan says: “Data is critical to enable us to hold that mirror up to see if we can do things more effectively. It gives us a much better understanding of what is going on, for example, have we really had 50,000 patient contacts in the last two weeks or is it 40,000 with the other 10,000 being patients trying to make follow up appointments? Are we creating demand because of the way we are working?”
Analysing data at that level can help surgeries to understand high intensity users, looking at those who have complex needs and seeing how they GPs can support them better.
By building collectively on an effective programme of change, supported by detailed data for improvement, the practices of Wigan are set to remain leaders in patient access to general practice.








