Digital Triage and Demand-Flow. EFPC Porto
Hypothesis: efficient operation of primary care depends on clinical triage of all demand, to optimise the use of scarce consulting resource – GP time.
The faster and simpler the system, the more patients will co-operate.
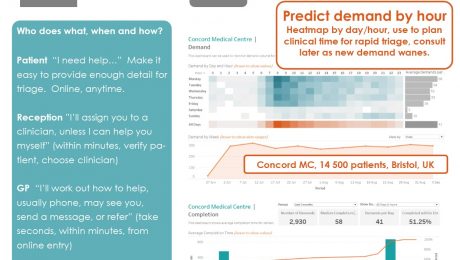
Who does what, when and how?
Patient “I need help…” Make it easy to provide enough detail for triage. Online, anytime.
Reception ”I’ll assign you to a clinician, unless I can help you myself” (within minutes, verify patient, choose clinician)
GP “I’ll work out how to help, usually phone, may see you, send a message, or refer” (take seconds, within minutes, from online entry)
Consult & complete – precisely appropriate for the patient and episode.
Presented at EFPC European Forum for Primary Care, Annual Conference Porto 24-26 September 2017
Download the poster here:
- Published in Evidence
Bad general practice is driving out good
Known since before Tudor times, named Gresham’s law in 1860, thoughtful observers have realised that “Bad money drives out good”. When two forms of currency are in circulation, the debased version quickly replaces that of true value. It’s happening now, paid for by the NHS, in general practice.
Oxford CCG proudly trumpets the big numbers, “15,000 extra GP appointments in £4m scheme.” Divide £4m by 15,000 x 12 months and we find the cost per appointment is £67. That’s over twice the fully absorbed average cost of a regular GP appointment.
It gets worse: regular GPs are funded by capitation, not by activity (per appointment) and their contract means they are already responsible for their registered patients who are or believe themselves to be ill. The CCG is paying £6 per patient for a service already fully funded – it’s paying twice. But not the CCG – it comes from an NHS England pot, descended from a GP Access fund which covered less than 10% of England – a lottery as to whether your area is included.
It gets worse: a GP federation officer says it’s for those patients having to wait 2 to 3 weeks to see their own GP. These GPs are failing their patients with an appalling service. They are being rewarded for failure, incentivised to fail more as worse access will move more of their patients into the “extended service hubs”. Patients at GPs offering an excellent service, such as Oak Tree Didcot which we helped over 5 years ago, have no need and no desire to travel further to see a doctor they don’t know.
It gets worse: my Didcot GP friend tells me “it is virtually impossible to find GP locums or recruit GPs because many are now working in these hubs seeing relatively straight forward problems, with 15 minute appointments, whether the patient needs 15 minutes or not.” [and we know that utilisation of slots is low, many will be left empty]
All right thinking people can see this. So why is it happening? Control of the money lies with those who don’t want to see: NHS England, who knows why, Oxford CCG who think they have a “nice” headline, and the GP federation owners so happy to take up the offer of highly profitable light duties. £4m will get soaked up in a year with no difficulty at all, and when the money stops, so will the service. This is the very antithesis of sustainable continuous improvement.
What can you do? Fight this debasing of general practice with every bone in your body. The RCGP, BMA and all in leadership positions should be calling this out. Local GP Dr Helen Salisbury says, “It might be better if we could just fund GPs properly,’ Too right. NHS funding must go to where it is of highest quality, most effective and productive, core general practice.
I don’t like to end without hope, because we need hope, and Gregory Bateson’s analogue is worth noting: “the oversimplified ideas will always displace the sophisticated, and the vulgar and hateful will always displace the beautiful. And yet the beautiful persists.”
Fight for the beautiful.
Harry Longman
PS last week’s launch in Surrey has gone well, GPs dealing with all demand on the day, patients amazed. A couple of examples stood out for me on day one: the lady who walked straight to the desk at 8:35 expecting a queue of 10 and a rammed waiting room: nobody. Look of total bewilderment – “are you open?” And the patient late in the afternoon who, on the way out, stopped at reception to thank the whole team for the wonderful service she’d had. Gets me out of bed every morning.
- Published in Comment
Fancy a 10 hour working day?
I do hope you are thoroughly refreshed and have enjoyed the break from my blog. I mean your work. Oh, whatever, I’ll stop digging.
But I wonder how you view the thought of a 10 hour working day? Horror or relief? It’s relative isn’t it, because to some that would be 2.5 hours over the regulation 7.5, to others it might bring sanity at last to a regime which has been 12 or even 14 hours. People aren’t made for that and whatever you earn, it can make life not worth living.
So I was struck when a GP partner recently said she had this burning ambition for a 10 hour day, when completing our Could you be ready to change? (we do this with everyone thinking about system change. Nothing matters more than having a burning ambition).
Reducing GP workload has been number one topic in Pulse, BMA, RCGP and goodness knows where else, and the bad news is that we can’t wave a magic wand to reduce it. There are lots of factors. One is patient demand, which is remarkably constant, whatever we do. It isn’t going up, though revisiting a Liverpool practice we first helped five years ago is encouraging – demand is down 10%.
But what we can do, and to some this does seem like a miracle, is dramatically improve efficiency. It’s intense, and getting it right means careful analysis of consultation times, modes, referral and resolve rates, but it does work. Unmet demand is a factor, and simply meeting this can soak up a proportion of time freed up by a 20% efficiency gain, but almost always there’s plenty left over for getting the hours down.
Efficiency is our absolute laser focus – how you convert that to your benefit is up to you.
Overwhelmingly GPs tell us “I feel more in control”, as another partner did last month having launched in June, and it’s the control that makes work satisfying, even though it can be intense.
We love what we do and those kind of comments get me out of bed every morning. It will be an early start Monday to be at our first autumn launch in Surrey – I can hardly wait.
Harry Longman
- Published in Comment
Happier GPs?
Are you enjoying the Proms? I’ve only been a couple of times but I love the wealth of music on offer, some familiar, some challenging.
David Sawer’s “The Greatest Happiness Principle” and the Proms Extra talk got me thinking last Saturday. We put “Happier GPs” on our askmyGP home page, because it’s a direct quote from GPs. But what might that mean? A non-stop cheesy grin, I think not.
The evidence is that we don’t consciously think of ourselves in a state of happiness (the strong conscious emotions are the negatives), but we are living in the moment. Contributors include:
- doing something good for others
- flow, being totally absorbed at the limit of our capability
- control of our own time and efforts
It isn’t the same as an “easy life”, pleasures with which we may relax but too much of which don’t give us meaning. So we aren’t saying to GPs, put your feet up, but reflecting the kind of things they say. Last week I was in a practice where one partner reflected “I feel so much safer now” (they are dealing with all demand same day, where it had been only 40%).
In another, the manager said last Thursday they had all finished by 4pm so they went home except for the one on duty, who dealt with five calls before 6.30. That’s not every day, but most GPs would have a clinic full of patients booked three weeks ago who may or may not turn up. In contrast, knowing you are providing a fabulous service and can have that flexibility is enormously liberating.
You don’t need me to tell you that the narrative in the medical press is so different, and BMJ front page last week has BURNOUT in big capitals. But the editorial is right on the mark: “Solutions have traditionally focused on individuals and their resilience.” whereas, they continue, “A systems level approach is imperative…”
We couldn’t agree more. It’s the system.
Regards,
Harry Longman
PS this makes me a little bit happy, the first askmyGP feedback at 8 this morning, “I really like this new service and I cannot say enough how much easier this is to access medical treatment. The surgery is fantastic.” This theme is so often repeated that it’s getting boring. The meaning for me comes in asking, “How can we multiply it by ten thousand?”
- Published in Comment
How to count sheep
When I was five I used to love asking my farmer uncle how he counted his sheep. “Count the legs and divide by four” he was sure to reply, and I was sure to giggle. Thanks Ray, for the laughter and learning you sparked.
Measurement, a kind of counting with maths, is a huge part of what we do and we are always trying to make it simpler and clearer.
The simplest, most important measure in general practice is demand – by month, week, day, hour.
Then comes the service response – how fast, how soon? That’s what matters most to patients. Why isn’t anyone else doing this?
Then comes efficiency – how long does it take to deal with all those demands? That’s what matters to GPs and staff – they want a reasonable working day, and without harming patients improving efficiency is the surest way.
All these are operational measures we derive on an industrial scale with minimal effort and immediate visibility.
So It grieves me to see hundreds of £k spent on fiddly little “improvements” which make no attempt to measure benefit for patients. They trumpet thousands of hours saved – which turn out to be approximately 17 minutes per GP per week.
It grieves me to see the vast expense on poor substitutes for measures, postal surveys with small samples and smaller response rates, reported months later. Counting legs.
It grieves me to see the BMA making threats to close GP lists, unable or unwilling to frame questions of capacity in terms of efficiency.
When you make a step change in efficiency, lots more becomes possible in ways we can’t measure with numbers.
Read in Pulse how Dr Steve Edgar describes “Taking back control”, using terms like autonomy, mastery and purpose, with time for the simple team huddle.
If you’re heading to the hills this week you’re sure to see a few sheep. Yan, tan, tethera…
Regards,
Harry Longman
PS Reminder of the poster study of online consultations at Concord Medical Centre. Another step on the efficiency road.
- Published in Comment
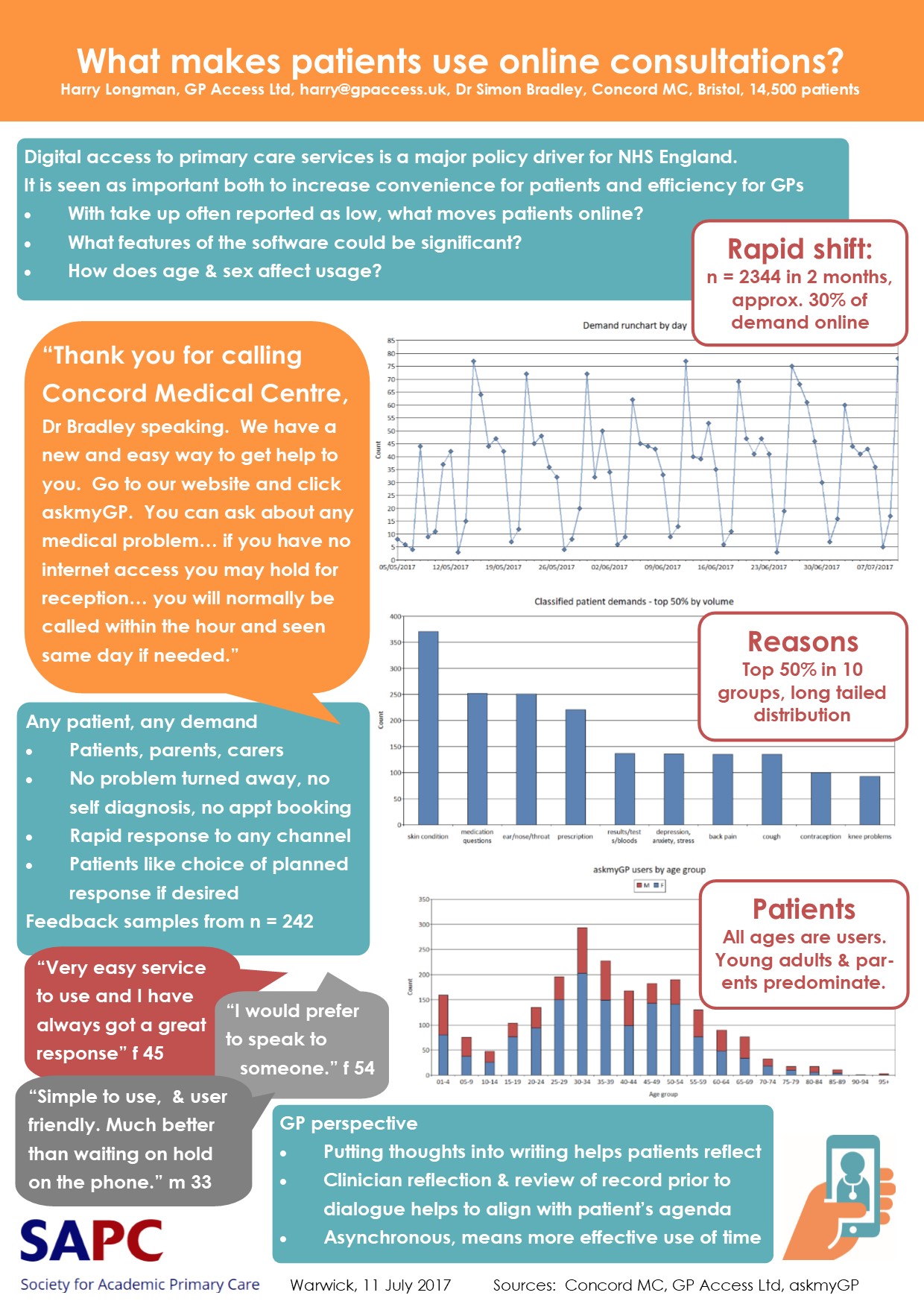
SAPC Poster: Moving patients online
A quick note with exciting news, we’ve just had our poster published at the Society of Academic Primary Care SAPC Annual Scientific Meeting in Warwick.
askmyGP has now passed over 50,000 patient episodes, 4,000 of them on the all new platform launched just two months ago.
The case study with Concord Medical Centre, Bristol, is here:
What Makes Patients Use Online Consultations
What took demand to 30% online? In a nutshell, it’s:
– Personal (“Hello, I’m Dr Bradley…)
– Universal (all patients, all problems)
– Responsive (we’ll get back within the hour)
– Simple (“Easy to use” main theme of feedback)
We took the decision in version 2 to take OUT the clever technology we’d put in v1.
It’s much simpler, with the aim of putting patients in faster, easier, touch with their GP, and vice versa. It builds trust by allowing patients to express exactly what they mean.
The result? Positive feedback has shot up, both from patients and GPs.
Dr Simon Bradley comments:
“The thought that goes into putting something into writing often helps the patient to have reflected on their problem prior to initiating a request.
Then for the clinician to have reflected on the request and reviewed relevant elements of the record means we can be more aligned with the patient’s agenda.
Online communication is asynchronous which allows both patient and practice to use their time more effectively.”
Aha. Time. The only absolutely finite resource.
Time for recreation too – enjoy the weekend.
Regards,
Harry Longman
Download pdf: What makes patients use online consultations?
- Published in Evidence
Surfing the demand wave
Summer may be a-coming in, we will see beaches and I promised to take a look at that pattern of patient tidal flow.
GP demand is like a rolling wave. Or quite like a skijump, or one side of a volcano, but let’s stay with the wave for the purposes of surfing.
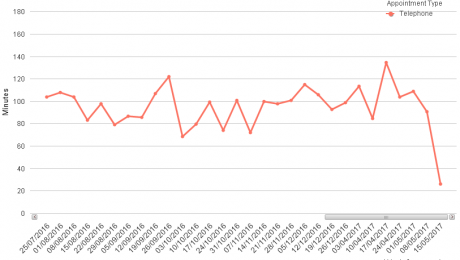
We’ve analysed hundreds of practices and when you allow patients call any time in working hours the pattern is strikingly similar across the board. The calls start high when you open at 8, stay there for a short time and from 9 fall rapidly through the morning. They flatten out through the middle of the day and early afternoon, then tail off from around four down to very little by 6.
Aha. So how to respond?
- Tidal deniers: “We hold our partnership meetings at 8.30 on a Monday morning. Works well for us as everyone is in, perfect start to the week”. If only they spent five minutes in reception.
- Tidal self harmers: “Sorry, what do you expect, it’s already 8.17 and there’s nothing left. Call back tomorrow but make it early I should to be sure of an appointment” Funny how every day is the same.
- Dudes: we’re ready, on it as the demand comes in, phone or online first response, deal with it now, decide to see some later when incoming is quieter. Stay on the wave, take a break, mentally prepare for face to faces, back for next session. It’s a full on day, but we feel in control.
Someone accused me on Twitter this week of common sense and I strenuously deny all charges, but really, is it that hard? So why do patients wait an average of 5 days to get help from their GP? And why do GPs end the day shredded?
One practice we’re working with has hit a median response time by a GP to any patient demand of 17 minutes. Within five weeks of launch. 17 minutes. Surfin’
Harry Longman
askmyGP & GP Access Ltd
PS Delighted to see that Matthew Swindells, new Director of Operations at NHS England, is starting to call out NHS111 for the monstrous waste that it is. Sad to say that it’s taken a change of personnel to admit the truth, while those four years have seen hundreds of £m wasted, never mind the frustrations for patients, GPs and staff. So will he actually do the necessary?
- Published in Comment
Is there a crisis in clinical consultations?
Quite a week but let’s put all that to one side and reflect on a fabulous article I came across, which put into perspective what we are trying to do.
Dr John Launer of HEE asks Is there a crisis in clinical consultations? Although he sets the paper in a hospital context, most of his working life has been in primary care and the same principles and questions apply. It’s all about
“the idea that making it easier for clinicians simply to talk with patients may solve many problems that managers might assume need far more complex technological solutions”
Aha. Let’s add to that the assumptions of politicians, along with structural, financial and all kinds of other complicated solutions.
Launer quotes Dr Gordon Caldwell who has outlined ten fundamental conditions to optimise consultations, including:
- The patient should be as prepared as possible
- The clinician should be as prepared as possible
- Ready supply of information into the consultation
Telephone consulting pioneer Dr Steve Laitner contrasts traditional general practice in a tweet, “like having a day of back to back meetings every ten minutes with no idea who you’re meeting and no agendas”
Stressful and far less productive than it might be.
Yet patients are willing to spend their own time writing and preparing when they seek help – we need the system to make it available to GPs.
A recurring theme of patient feedback on askmyGP is “I was able to gather my thoughts before seeing the doctor. I so often forget things when I’m in there.”
Clinicians value enormously what patients write, whether preparing for a phone or face to face consultation. Our task is to develop the handful of questions which provide the most useful information, and I’m delighted to say that researchers are interested in this too.
Our other focus is to make online access so easy and attractive that it becomes the norm. We are over 30% in one practice and it will take a lot of experiment and refinement but I’m looking forward to reaching 50%, which I hope will make a big contribution to clinical quality.
I’ll leave you to look up all ten principles in Launer’s article, but here’s one you will like: “The clinician should be regularly refreshed”. He doesn’t say what with.
Harry Longman
askmyGP & GP Access Ltd
- Published in News
What’s your DNH rate?
OK, you’re forgiven for thinking I wrote DNA rate, and you were expecting to read about how to reduce Did-Not-Attends, perhaps a mix of clever texting apps and a patient blame-fest of warnings, charges and excommunication. No matter, although we have shown that DNAs are a system problem, not a patient problem, and if you change the system, DNAs disappear.
I wrote DNH meaning Did-Not-Help, the patients who are told by reception, “Sorry, nothing left, call back tomorrow. And make it on the dot of 8, I should, we’re very busy.”
No clinical systems measure this, NHS England would rather ignore it, no political party understands it or has the method or means to deal with it. The various prescriptions of “waiting time targets” or “8-8 x 7 day opening hours” aren’t based on examination of the evidence, so the diagnosis is wrong and the treatment will fail.
We collect the evidence through our Datalog audit, real time, patient by patient, we have n > 300,000 from over 200 practices, and the average rate is… 12%. Yes, it’s roughly twice as high as the average patient DNA rate, and it’s not caused by patients but by GP practices and systems. The highest we’ve measured in any practice is a staggering 31% of demand turned away.
I’ve worked with enough GPs to know that the vast majority joined the profession to help patients, so the data may come as something of a shock, but something which should move us to action. True, there’s a small but powerful minority who seem to take a different view, maximising profit by minimising service to the point where they just escape being caught.
But we are concerned with the vast majority, those working hard to provide excellent patient service. Getting GPs to work harder is a sure fire vote loser, I think you know that. So the answer is giving them the method and means so that they can work much more efficiently, dealing appropriately with all demand and feeling in control.
Our task in fulfilling the vision “to transform access to medical care” is working out ever better ways to make this happen. We know that dreaded phrase, “Call back tomorrow… ” is uttered around 100,000 times per working day in the UK and our manifesto is to eliminate it.
You will vote many times in your life. Make your vote count.
You will live only once. Make your life count.
Harry Longman
Founder, Chief Executive, GP Access Ltd
PS Exciting to report that the next little piece of that road is now in place, two way secure messaging between GPs, their staff and patients. It enables more efficient use of GP time by not always having to find phone numbers and hope for an answer. Spoke to one user yesterday who already loves it after sending 3 messages! It’s built into askmyGP Transform and Improve.
PPS as election guide I defer to the inestimable @jtweeterson
@harrylongman
- Published in Comment
It’s lovely not being shouted at 24/7
“It’s lovely not being shouted at 24/7”
Receptionist Karen’s first comment to me was both startling and predictable. Her Somerset practice launched their demand led system two weeks ago, and since then she has been able to help every patient. Three weeks ago she and her colleagues were turning away one in five patients (we measured it) but they have moved straight into the super league, with a median response time from the GPs of 26 minutes.
The GPs love it too, but I find they are more buttoned up and try to find at least one thing to grumble about. “I’ll be home early so will have to put the kids to bed,” said one.
That didn’t take too long did it, or seem so hard? It was four weeks of preparation, to abolish the old system and start the new.
So why aren’t we hearing about this from the commentariat? I get a stream of dismal blogs from Nuffield/King’s Fund/Health Foundation (why don’t they just merge, it would save all those personnel transfer costs?) wringing their hands about how hard it is to change anything.
Another one today on General Practice at Scale, is it working? Yawn. Fiddling with structures, the obsession of policy makers who should get out more and ask “WHAT WORKS?”. Instead we’re told,
“Motivations… centred on a desire to offer better access…
Most strikingly, what the survey revealed was just how long enacting change can take – at least two years to even begin to achieve what they’d set out to do.”
Useless. And no measure of performance is even offered. This is why Deming said that motivation is fine but worthless on its own. The question is “By what method?”
Method is central to our work and it’s so repeatable now that the outcome is binary: either the practice decides to change, and it all happens within a month, or it doesn’t, and nothing much happens at all, ever.
But method is not static, we are continually learning and having to adapt. Another Midlands practice told me yesterday they are learning lots from having a GP in reception, sometimes even taking calls from patients, and their performance is rocketing while demand is falling.
I’m not going to call it a trend yet, but if you are a demand led practice you’re probably enjoying the sunshine dividend today. Have a great weekend.
Harry Longman
PS Learning a lot from askmyGP users too, with over 1200 episodes and 130 patient feedbacks on the new system, 55 suggestions from staff, a terrific response. We’ve already put dozens into service and next week’s plans include one for low using practices (they will get an email notification of an online demand) and one very much anticipated by high users.
GPs have been emailing patients because it’s convenient – but it’s not secure and poorly controlled for IG and patient safety. From next week those on the Transform programme will be able to securely message patients in a two way conversation. It’s going to be another huge time saver. Will let you know how it goes.
- Published in Evidence