Wigan Borough CCG improves patient experience and builds capacity
How an online total triage solution improved patient experience and is helping to increase capacity – Jonathan Kerry, Associate Director of Primary Care explains
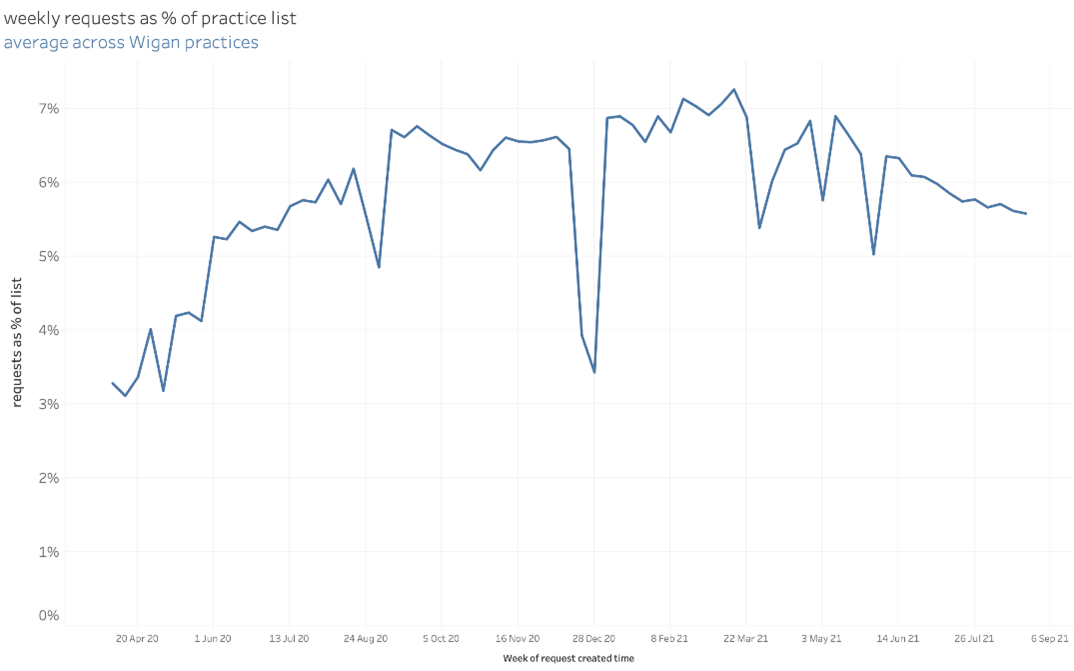
NHS Wigan Borough CCG has 58 GP practices varying in size from small to large. One of its larger practices has a patient list of 17,500 patients, while the average is around 5,000. Until the COVID-19 pandemic hit, just a handful had made the switch to digital working and total triage solutions. However in March 2020, when the doors shut, most practices faced a rapid implementation of digital systems to ensure GPs could continue to provide a service to their patients. The CCG recommended the askmyGP total triage solution and throughout the primary care networks (PCNs) practices started working together to learn from and support one another. Since then, the practices of Wigan have managed over one million patient requests via the askmyGP system, providing an extensive and robust dataset with which to improve ways of working. As well as improving the patient experience, data from askmyGP provides actionable insight, highlighting ways in which workflows can be improved by creating capacity and ensuring all patients are seen by the right person at the right time, while also helping to relieve the significant pressures currently being felt by GPs.
Standardisation leads to greater collaboration and new ways of working
When the COVID-19 pandemic took hold, the shift to digital had already been specified by the CCG within its primary care contracts. Many practices were behind schedule, but consideration also had to be given to how a total triage system could take healthcare forward. The CCG wanted to look beyond the pandemic to improving capacity and access in the future rather than just being a bolt on option giving patients an additional way to book an appointment.
Jonathan Kerry is Associate Director of Primary Care for NHS Wigan CCG. He says the PCNs supported this approach while also encouraging as much standardisation as possible across the system. He says: “If you can standardise at PCN level it makes it easier for practices during a challenging time. Even if it’s just sharing staff and providing resilience these are still worthwhile benefits.”
The push for standardisation was successful. Currently there are 43 practices out of 58 using askmyGP, giving 24/7 access to GP services. Jonathan says: “It helps to identify who is in most need, those who might need face to face or a different type of consultation method.
The PCNs supported standardisation between practices by creating working group forums, aiding learning about how askmyGP can be used to increase efficiency and make positive change. Having already worked together in the form of neighbourhood clusters since 2013, there were ready-made working groups for many clinical leads such as practice managers and nurses as well as patient forums.
Bringing everyone together to discuss any challenges or concerns meant that it was possible to take insight from askmyGP and create an action plan for change. Key to the success of the system is being able to offer core GP services and 24/7 access, but also helping patients to understand if other services can provide the help they need.
A recent snapshot survey by Pulse has revealed that waiting times for GP services across the UK came down during the pandemic as a result of online triaging and remote consultation.
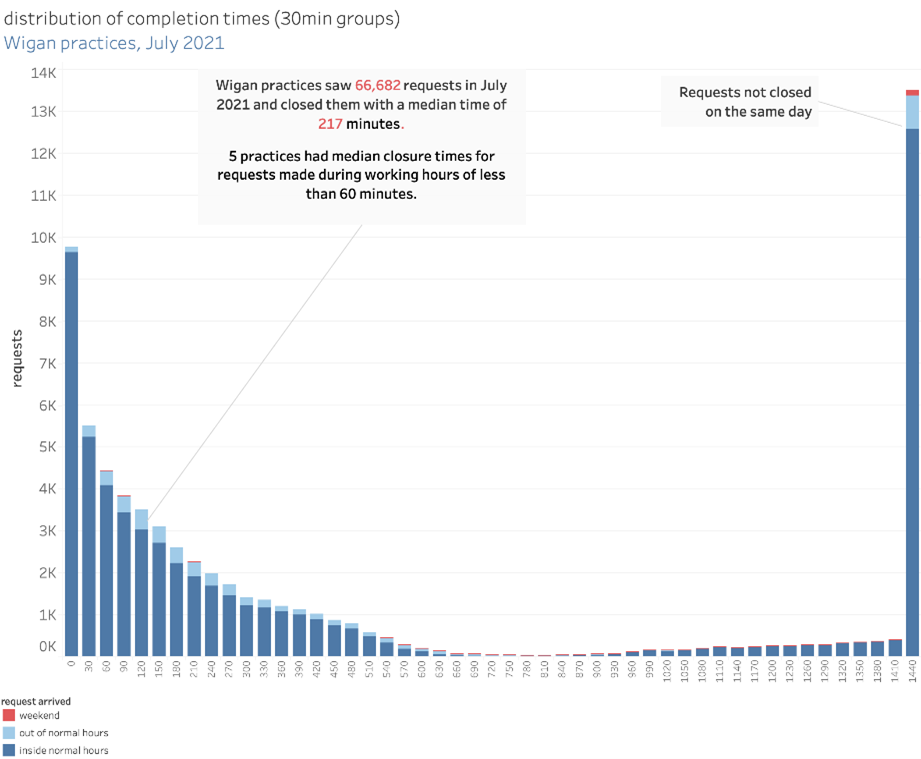
The findings from May reveal the average waiting time for a non-urgent in-person appointment following triage is down to 8.7 days, while the average wait for a phone or video consultation is 7.4 days. GP practices in Wigan using askmyGP have achieved a median waiting time of just 217 minutes.
However demand has risen, and GPs are doing more consultations than ever, creating significant pressures. By having several surgeries operating from the same system, it can mean sharing responsibilities rather than having all those surgeries simply replicating the way they work.
For example the PCNs in Wigan CCG have collaborated with a First Contact Physio initiative, which aids triage, helping to signpost the patient to the most appropriate person, rather than automatically seeing the GP as the first port of call.
Jonathan says: “It may not be a physio, but a social prescriber or community link worker. We just need to be able to get patients to the person who can help them and support them best. We can use the technology to underpin that and support them.”
“This is a good example of how to start, it was a rapid implementation to help practices during the COVID-19 pandemic, but the way that we are using First Contact Physios shows the potential and longevity of that way of working.
Expanding capacity and creating new ways of working
The introduction of online triage has been a broadly positive move for patients.
Feedback from the Friends and Family Test has been significantly higher than it has ever been. Over the last 12 months ratings have ranged from 75 to 90 per cent of people saying the service has been better or excellent compared to previous visits. “From a patient point of view, generally there is real positivity for it,” says Jonathan.
There are also encouraging signs from the National GP Patient Survey, taken in the first three months of 2021, which has shown the CCG area to be higher than average in its use of digital and around access to GPs.
However, Jonathan acknowledges that, while online triaging can be extremely positive for many, there is the potential that it can exacerbate inequalities. He says: “This is something that is always going to be there, so we have to keep working at it and making sure we are doing the right thing.”
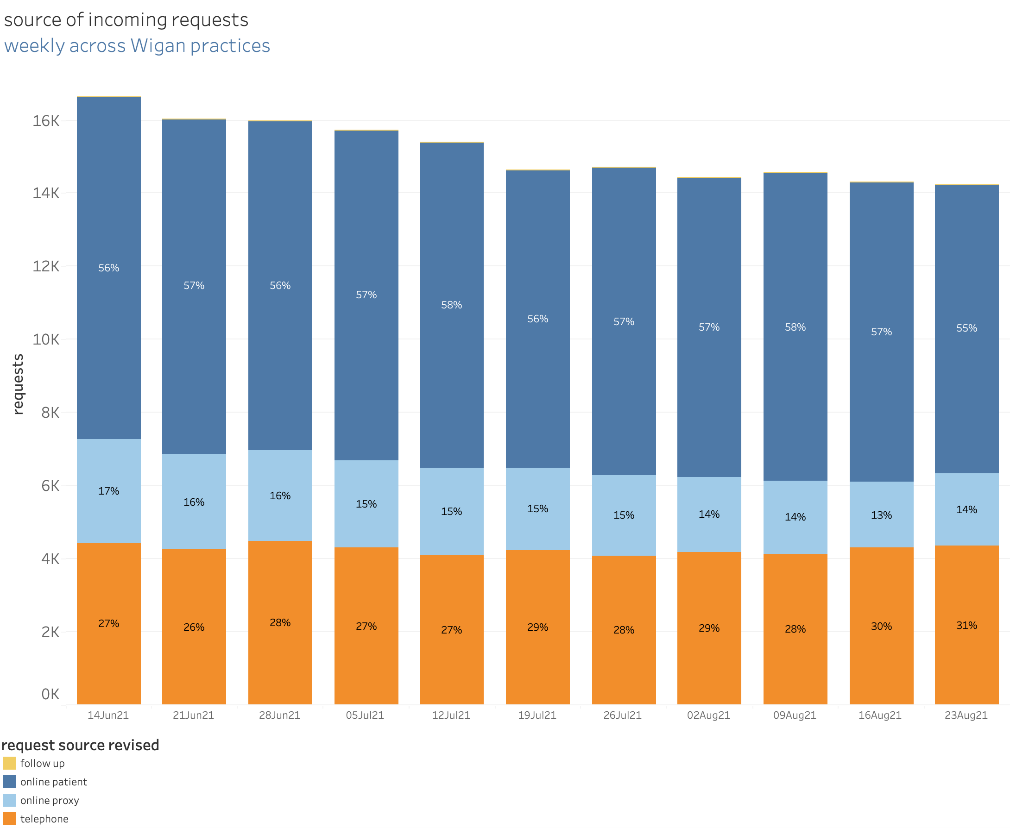
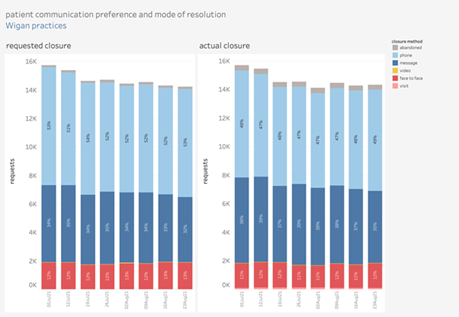
With askmyGP, patients can choose their method of contact. If they’re not online, the system is set up to ensure they get the same service should they need to phone the surgery or go in person. No-one should ever be forced to use the online system if they don’t want to.
The CCG is currently carrying out market research looking in more detail at the expectations of patients. Speaking to around 3,000 people, the CCG will formulate patient models to help them better understand patient need and see how they can evolve over the next decade.
Regular data can help surgeries hold a mirror up to the way they work
askmyGP generates data daily that can help practices track how they are working and focus on where change needs to be made. The data shows how the system is being used and the mechanisms which patients choose to make contact along with the reasons why.
Jonathan says: “Data is critical to enable us to hold that mirror up to see if we can do things more effectively. It gives us a much better understanding of what is going on, for example, have we really had 50,000 patient contacts in the last two weeks or is it 40,000 with the other 10,000 being patients trying to make follow up appointments? Are we creating demand because of the way we are working?”
Analysing data at that level can help surgeries to understand high intensity users, looking at those who have complex needs and seeing how they GPs can support them better.
By building collectively on an effective programme of change, supported by detailed data for improvement, the practices of Wigan are set to remain leaders in patient access to general practice.
- Published in Case studies
How askmyGP is providing a system that works for everyone at The Grove Medical Centre
Summary
Over the past year, many GP practices have turned to askmyGP to help them navigate the challenges the pandemic has presented. The Grove Medical Centre in Swansea, which covers a patient population of approximately 7,500 people, has been using askmyGP since April 2020. We spoke with Dr Jack Williams, one of the four GP partners at The Grove, about his experience of the system and the benefits it offers the practice.
Triage system working for all types of patients
Before the pandemic, the system in place at The Grove ensured patients always experienced excellent availability of appointments, with almost all patients being seen on the same day they requested an appointment. There was no triage system in place as there was no need for one. When Covid-19 began to surge in the UK, the practice team decided that a triage system would be vital to maintain the quality of service and for the safety of patients and staff. Following a short implementation period, The Grove launched askmyGP at the beginning of April.
The team wasn’t sure how patients would take to it, but the initial feedback they received was very positive. Dr Williams says: “What we found was that it was actually a very good time to implement a new system because the pandemic meant people were more accepting and understanding of the need to change.”
The Grove has a wide patient demographic, with many different ages and levels of deprivation represented. The practice has found that most people have been able to use the new system with no problems, with the data showing that even patients over 90 are accessing the practice online.
The practice expected a small number of people would still need to access the practice via phone, however, as Dr Williams explains: “We are encouraging people to go online, but that is not a barrier – we knew there would be people who don’t have access to the internet and these patients tend to be our more vulnerable members of society. The phone lines are still open, and in fact askmyGP has benefitted these vulnerable patients by making our phone lines less busy for them, so those that do call find it easier to get through.”
No effect on clinical judgement or prescribing activity
An area of concern around the increased use of digital tools such as total triage and remote consultations has been the effect this may have on clinical prescribing behaviour. Health Foundation research, however, found no significant evidence of the askmyGP model affecting prescribing rates. This aligns with the experience of GPs at The Grove Medical Centre.
Dr Williams says: “For us, it’s not all about e-consulting. Yes askmyGP allows us to e-consult, but the benefit for us is that it is a triage system with the capability to do an e-consult if we wish. We can respond to people with a message on the system, but we will still call the patient or conduct a patient examination if needed. We are conscious not to allow these new ways of consulting affect our clinical judgement and our data shows that we actually see more patients face to face, than are requesting this type of consultation.”
Matching demand and capacity to ensure requests are resolved quickly
The practice team was keen to ensure that they were able to continue resolving as many requests as possible on the same day they came in. The data askmyGP provides The Grove shows that requests are resolved on average 116 minutes after they were made. The data also enables a more proactive approach to staffing, as the practice is able to predict demand at weekly, daily, and even hourly levels.
This has been enormously helpful during the pandemic, says Dr Williams. “The visibility of demand that askmyGP offers has enabled us to rearrange rotas and match our capacity to that. This also helps with staff morale, as it means we can aim for all the staff being equally busy on different days.”
Image: Swansea Marina © Crown copyright (2013) Visit Wales
- Published in Case studies
Weston askmyGP Case Study
In September 2018 a year-long project was initiated by the local CCG to support recruitment and retention in Weston-super-Mare, which has the highest proportion of GPs and nurses in the CCG area nearing retirement.
With significant demographic pressures from a population that is both ageing and growing, practices in the town and surrounding villages were under severe pressure with an unsustainable workload. Many practices were relying on locum doctors to fill sessions.
With askmyGP fully implemented at New Court Surgery life for the practice team has been transformed. Patients contact the practice by phone or via the practice website, with all requests processed through askmyGP. Doctors review all requests and allocate them to the most appropriate team member to deal with.
Dr Heather says: “There has been a massive improvement in the flow of patients through the surgery and patient satisfaction is generally very high. The clinicians are more in control and we are able to deliver good access alongside great care.
Read more in the case study: NewCourt
- Published in Case studies
“Do you shop online?” Rural Ruskington GP moves 80% on day one
The staff room looks out over fields, a couple of hens pecking in the long grass over the fence. We’ve driven Lincolnshire’s challenging roads and arrived through quiet village streets and bungalows. Think everything Salford isn’t: elderly, stable, families and retired.
The new record set by Ruskington Medical Practice was to abolish the old and launch a completely new system from receipt of order in just ten days.
It’s the last place in the UK you’d expect to see this, but from day one they have got 80% of demand online.
They know that almost everyone under 65 has online access, and a large proportion of much older patients. The patients haven’t yet realised there’s an easier way to get help, so if they ignore the GP recorded message, the receptionist asks:
“Do you shop online?”
That simple question, almost always answered yes, means they can be directed to the website (or sent a welcome email) and off they go. Request arrives online, it’s sorted to the appropriate person, and completed within a median 91 minutes. Only 23% need a face to face or visit.
Credit to practice manager Jules for that phrase – we love simple. She’s happy, staff are happy, GPs happy, and patient feedback shows 78% say the new system is better (one aged 90), only 12 days in.
Jules tells me demand is below prediction, which I find slightly annoying as we do like to get this right.
I’ve counted and “Do you shop online?” has exactly half the syllables of “Patient Communication Strategy”. It would be funny if it wasn’t sad, but NHS England’s Patient Online programme has taken 8 years and spent countless £millions of taxpayers’ money on telling patients to book appointments online, and they’ve reached 4%.
It hasn’t worked and it will never work because GPs are smart enough to realise that allowing patients to book all their time will waste a good 2/3rds of it.
Here’s the offer that works for patients:
Tell us who you are and what is your problem, and we’ll work out how to help you. Boom.
You’d be amazed how many times GPs tell me “this wouldn’t work for our patients” – perhaps because they’ve tried something which didn’t work. That is why simplicity is so important, and why Computer Must Never Say No.
Ruskington at 80% still welcome those with no online access. Suburban Hounslow is another new launch, 86% online, Salford remain highest at 98%.
We’re looking forward to a Surrey commuter practice making the last launch of 2019 on 23rd December, and a Lincs seaside town the first of 2020 on 2nd January.
Never know who might set a new record…
Harry Longman
PS Often a fear of “opening the floodgates” leaves people torn about the risk of change. In the recorded webinar Understanding Demand we examine the evidence of what happens. Free to register.
For an idea of how the askmyGP could put you in control of your day, click here to get our four user stories.
- Published in Case studies
Digital First GP: Blackfriars Salford gets 97% online
The walk down from Manchester Piccadilly is a fascinating cityscape, and then crossing the river Irwell into Salford it seems everything is in flux.
Here, between the £180/night Lowry Hotel and the £35/night Salford Arms Hotel, lies Blackfriars Medical Practice. Perhaps that’s a metaphor for the patients Dr Babar Farooq and his team serve: young, mobile, diverse and with fortunes right across the spectrum.
It’s free to join his list and free to get help – the NHS is a great leveller.
What’s unique is that when Blackfriars launched askmyGP three weeks ago they moved 97% of their patient demand online, from day one.
There’s no messing about – Linda on reception simply tells the patients what they need to do. They send online, they get sorted within a few hours (median time to complete the episode is 193 minutes). Computer never says no.
Inside the practice with the phone not constantly ringing the drop in stress and pressure is palpable. They are bouncing. Babar keeps telling me how happy he is, and he’s resolving 38% of requests simply by message.
Patients? 86% say the new system is better. “I was surprised at how quick my question was responded to. Much faster than calling.” is a typical response, female 29.
Their demographic is young, mostly 20s and 30s, so we wouldn’t expect every practice to get this many online, 80% would be more reasonable for the average normal digital first GP.
Blackfriars in week 3? They’ve just ticked up to 99%.
Harry Longman
Pictured, between the yellow sign and the railway bridge, ground floor.
- Published in Case studies









