BJGP: Patient use of an online triage platform, evaluation of askmyGP v2
We’re delighted to inform you today of the open access publication from Abi Eccles et al:
“BJGP: Patient use of an online triage platform”
It’s the first independent study of askmyGP and it’s well worth reading in full. I will quote the conclusion briefly:
“Patterns-of-use and patient types were in line with typical contacts to GP practices. Though the age of users was broad, highest levels of use were from younger patients. The perceived advantages to using online triage, such as convenience and ease of use, are often context dependent.”
What comes through for me is the very ordinariness of the online demand. It’s the same as normal demand, same patients, same conditions, same frequency by day of week and time of day.
There’s more on patient feedback too, with themes extracted which are very familiar to us. We’ve quantified the age question in our study on “Age specific adoption of online consultations.”
What this study adds is online usage orders of magnitude greater than any previous paper, with 5447 patient episodes from 9 practices in 10 weeks. Data collection was May to July 2017, which was our previous version 2 platform. Since then the same principles have been carried forward to v3 with a new design and many more features. Growth in usage means that we are now collecting the same volume of data roughly every two days.
The scope for further research is increasing daily with an anonymised database of some 300,000 episodes, unique in general practice. If you’re an academic in the field, we welcome the opportunity to collaborate, particularly on studies of the GP practice as a whole, not just online components.
Benefits for patients and GPs are the product of system change.
Regards,
Harry Longman
PS See how patients interact with askmyGP on our Bramley Demo Practice.
To experience the GP side, start with our free online demo.
- Published in Evidence
Age specific adoption of online consultations
Context
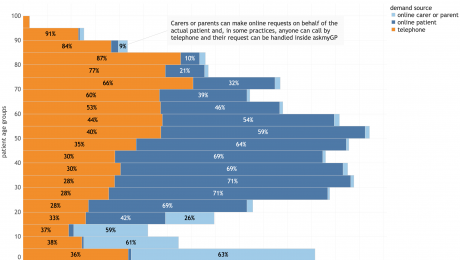
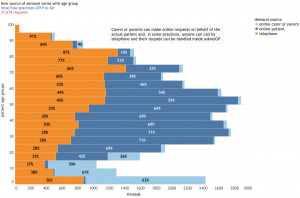
The latest data from our chief analyst Dr Steve Black (@sib313) shows remarkable adoption of online consultations across all ages and 10 diverse practices. n = 37,674 requests, date range is 1/1/2019 to 8/2/2019.
The context is all askmyGP practices operating in “total flow” mode where all patient demand goes through the system in two modes. Online, patients submit a request for help from their NHS GP practice either for themselves (dark blue) or as a proxy (light blue), mostly children but also vulnerable adults, most over 75. They may also telephone the practice, and a receptionist creates the request on their behalf (orange).
The key point is that all demand is covered in the chart, not from a self-selected subset of patients, and these are regular GP practices where there is no change in registration.
What the data shows
For infants and children, over 60% of parents chose to send their request online.
For young adults aged 20 – 40, over 70% submitted online.
With increasing age, the proportion online falls slowly, but even at 65 – 70 it is 40%.
Over 70 the proportion falls more steeply and significant numbers are by proxy.
Policy implications
It is clear that when designed for ease of use and universality in respect of patients and their medical problems, coupled with rapid response by providers, the online offer is highly attractive to patients.
The vision for “digital-first” providers who are at the same time traditional, local GP practices is achievable and already being achieved.
Harry Longman
Founder, Chief Executive, askmyGP
- Published in Evidence
Good news from GP patients
Good news has a hard time getting heard.
This week we’ve seen new, comprehensive data from NHS Digital on the wait to see a GP, splashed across all the papers:
Guardian: “One in five patients waits two weeks to see a GP”
Times: “Millions face a three week wait”
Telegraph: “One in ten waits three weeks to see their GP”
It’s all “true”, though I’m afraid the spin is not. The argument that “40% are seen the same day” rings hollow with anyone who has hung on the telephone for half an hour, to be told that all the same day slots have gone. Many of those 40% have been trying for several days just to get through.
Blame the patients, blame the government, blame whoever else we can think of. Or take a different look.
These tiny stories from the last few days are just a handful of the hundreds we see each week from patients grateful to their GP:
Your service and reliability are amazing. Thank you! (f 85)
Amazing fast system thank you (m 41)
Amazingly swift and very easy process than trying to jugggle around work – thank you so much! (f 24)
Amazing…More personal…Super speedy (parent, boy, 3)
Love how easy it is to speak to your own doctor . Amazing (parent, girl, 4)
Love this new system…so easy and quick , and have the problem solved without having to sit around at the surgery. (f 49)
Love ‘askmygp’. Making it so much easier to get info and solve problems whilst holding down a full time job! (f 40)
Wow. I am impressed! (m 69)
Wow, just wow. Have been in terrible painall night…absolute godsend… Thank you so much for your skills and innovations (f 65)
WOW, great system, quick easy, and no need to travel. Many thanks (m 63)
We’re now over 4,600 feedbacks from 80,000 episodes since August, and the trend is better and better. Please do have a look at the live rolling 7 day summary chart. We ask patients whether it’s better or worse and the ratio as I write has moved up to 9 which is so exciting.
These patients are getting an outstanding service from their own regular NHS GPs. The GPs have no extra funding (they pay us), and no complicated extended hours 8 to 8 hubs (that didn’t work)
Patients didn’t have to switch to an out of area GP. They could name their own GP. They were seen same day if needed.
And the GPs are happier too – happier professionally to be giving such a service and bringing the joy back into their working lives.
If you haven’t yet watched the Burnbrae video, please do and click for the demo at the end. This is one of her 5,000 patients last week, helped within 2 hours:
“fantastic service and Dr Arnott is an amazing doctor, Shotts is lucky to have all these new changes.”
How do we get this into the headlines?
Regards
Harry Longman
- Published in Evidence
You can’t please all of the patients all of the time
It’s remarkable for a quote that seems almost modern in politics, often attributed to Abraham Lincoln, but it seems he was quoting John Lydgate of Suffolk, writing in the fifteenth century, “You can’t please all of the patients, all of the time.”
OK he said people, not patients, but the point is made. You’d be mad to try and please all of the patients, all of the time, because whatever you do, some won’t like it, and that’s the thing about people. Perhaps that’s what makes us interesting.
Having said that, “Happier Patients” is one half of our motto and it is of utmost importance for us to do what is best for patients in the quality of service both we and the doctors provide. We ask patients directly for their feedback to help us achieve that.
In our version 2 askmyGP we’ve had over 4,500 patient comments from 105,000 episodes in the last 18 months. They have been overwhelmingly positive, with some negatives and some suggestions, and they have been a big part of our design process for version 3.
One difference is that where we used to collect feedback when the patient submitted the request, in the new version it’s done after the request has been completed. Ah, we thought, all those complaints based on the patient not believing it possible would vanish, and positivity would go up.
So far (first 4,000 episodes) it hasn’t quite worked out like that. We’ve structured the feedback very simply. The killer question is whether the new system is Better, Same or Worse, and the figures as I write are 98, 4, 27.
Yes, it’s overwhelmingly positive, and I’d love to share all the comments with you but even though we ask patients not to enter personal details, sometimes they do so we can’t do a real time feed. Some examples are below.
But I know what you’re thinking. I’ve been working with GPs for over nine years now and if I may be allowed a little over-generalisation, you’re really interested in the negatives. (btw academics are worse. They couldn’t find the silver lining in a solid silver tea service, present company excepted of course).
What’s interesting is that with the 21% who say it’s worse we are picking up reactions not only to askmyGP (though some are, and there were a couple of technical issues), but mainly to patients’ views of the GP. The main driver for negatives at 16/27 is very poor on “solving your problem”. It might be that something went wrong with the process, there was a delay, or the patient just didn’t like what the doctor said. Well, it happens, and you can’t please all of the patients all of the time.
Anyway, it’s good to see that 76% of those responding say the new system is better, while for those of you who think they are trumped by the 21%, you are amply justified in doing nothing.
Everyone can enjoy our star comment of the week, from a fellow Yorkshireman. This is only the opener and the rest has had to be moderated for family viewing, but you get the gist: “Whoever thought of this stupid idea wants a good kicking up the arse.”
Bless.
Harry Longman
PS Some of the feedback this week:
“Very good service it’s been amazing when I’ve needed advice for my children never waited longer than an hour for reply”
“far easier using this system than actually going through the surgery reception” male 28
“The new system is so much better, especially if you only want to ask a question rather than seeing a doctor. Massive thumbs up 👍” female 45
Thoughtful for others: “Ok for those who are familiar with the use of computer systems but I have concerns for elderly who would have no idea how to use a computer” female 70
- Published in Evidence
Digital Triage and Demand-Flow. EFPC Porto
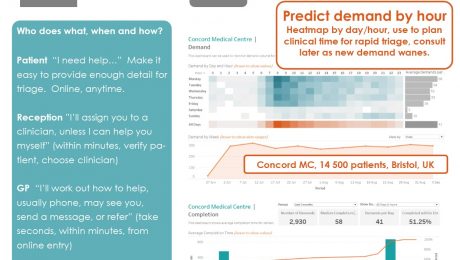
Hypothesis: efficient operation of primary care depends on clinical triage of all demand, to optimise the use of scarce consulting resource – GP time.
The faster and simpler the system, the more patients will co-operate.
Who does what, when and how?
Patient “I need help…” Make it easy to provide enough detail for triage. Online, anytime.
Reception ”I’ll assign you to a clinician, unless I can help you myself” (within minutes, verify patient, choose clinician)
GP “I’ll work out how to help, usually phone, may see you, send a message, or refer” (take seconds, within minutes, from online entry)
Consult & complete – precisely appropriate for the patient and episode.
Presented at EFPC European Forum for Primary Care, Annual Conference Porto 24-26 September 2017
Download the poster here:
- Published in Evidence
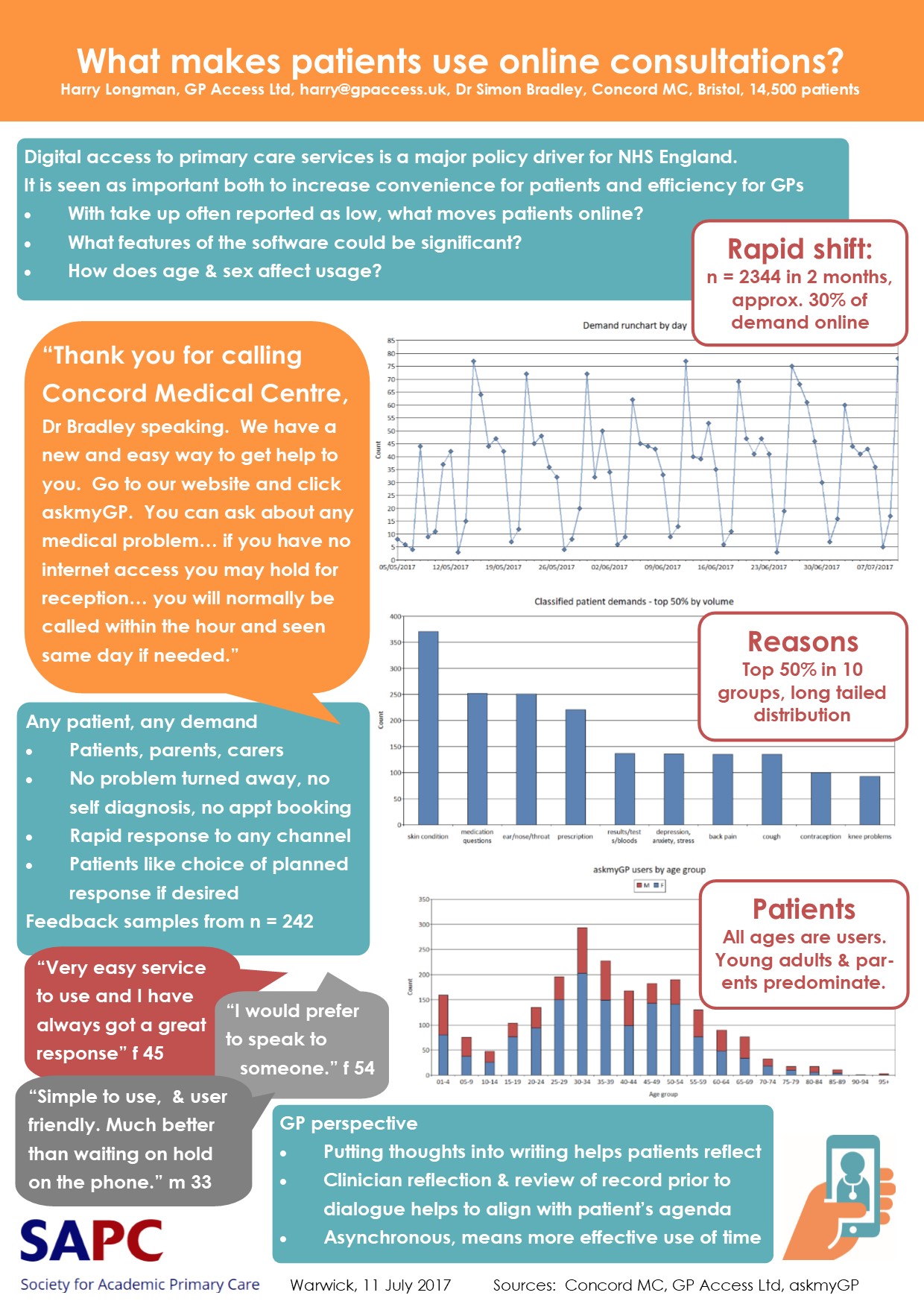
SAPC Poster: Moving patients online
A quick note with exciting news, we’ve just had our poster published at the Society of Academic Primary Care SAPC Annual Scientific Meeting in Warwick.
askmyGP has now passed over 50,000 patient episodes, 4,000 of them on the all new platform launched just two months ago.
The case study with Concord Medical Centre, Bristol, is here:
What Makes Patients Use Online Consultations
What took demand to 30% online? In a nutshell, it’s:
– Personal (“Hello, I’m Dr Bradley…)
– Universal (all patients, all problems)
– Responsive (we’ll get back within the hour)
– Simple (“Easy to use” main theme of feedback)
We took the decision in version 2 to take OUT the clever technology we’d put in v1.
It’s much simpler, with the aim of putting patients in faster, easier, touch with their GP, and vice versa. It builds trust by allowing patients to express exactly what they mean.
The result? Positive feedback has shot up, both from patients and GPs.
Dr Simon Bradley comments:
“The thought that goes into putting something into writing often helps the patient to have reflected on their problem prior to initiating a request.
Then for the clinician to have reflected on the request and reviewed relevant elements of the record means we can be more aligned with the patient’s agenda.
Online communication is asynchronous which allows both patient and practice to use their time more effectively.”
Aha. Time. The only absolutely finite resource.
Time for recreation too – enjoy the weekend.
Regards,
Harry Longman
Download pdf: What makes patients use online consultations?
- Published in Evidence
It’s lovely not being shouted at 24/7
“It’s lovely not being shouted at 24/7”
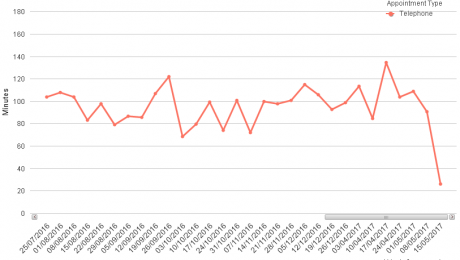
Receptionist Karen’s first comment to me was both startling and predictable. Her Somerset practice launched their demand led system two weeks ago, and since then she has been able to help every patient. Three weeks ago she and her colleagues were turning away one in five patients (we measured it) but they have moved straight into the super league, with a median response time from the GPs of 26 minutes.
The GPs love it too, but I find they are more buttoned up and try to find at least one thing to grumble about. “I’ll be home early so will have to put the kids to bed,” said one.
That didn’t take too long did it, or seem so hard? It was four weeks of preparation, to abolish the old system and start the new.
So why aren’t we hearing about this from the commentariat? I get a stream of dismal blogs from Nuffield/King’s Fund/Health Foundation (why don’t they just merge, it would save all those personnel transfer costs?) wringing their hands about how hard it is to change anything.
Another one today on General Practice at Scale, is it working? Yawn. Fiddling with structures, the obsession of policy makers who should get out more and ask “WHAT WORKS?”. Instead we’re told,
“Motivations… centred on a desire to offer better access…
Most strikingly, what the survey revealed was just how long enacting change can take – at least two years to even begin to achieve what they’d set out to do.”
Useless. And no measure of performance is even offered. This is why Deming said that motivation is fine but worthless on its own. The question is “By what method?”
Method is central to our work and it’s so repeatable now that the outcome is binary: either the practice decides to change, and it all happens within a month, or it doesn’t, and nothing much happens at all, ever.
But method is not static, we are continually learning and having to adapt. Another Midlands practice told me yesterday they are learning lots from having a GP in reception, sometimes even taking calls from patients, and their performance is rocketing while demand is falling.
I’m not going to call it a trend yet, but if you are a demand led practice you’re probably enjoying the sunshine dividend today. Have a great weekend.
Harry Longman
PS Learning a lot from askmyGP users too, with over 1200 episodes and 130 patient feedbacks on the new system, 55 suggestions from staff, a terrific response. We’ve already put dozens into service and next week’s plans include one for low using practices (they will get an email notification of an online demand) and one very much anticipated by high users.
GPs have been emailing patients because it’s convenient – but it’s not secure and poorly controlled for IG and patient safety. From next week those on the Transform programme will be able to securely message patients in a two way conversation. It’s going to be another huge time saver. Will let you know how it goes.
- Published in Evidence
Dutch study shows 12% demand reduction
“When the Facts Change, I Change My Mind. What Do You Do, Sir?” There’s a lengthy discussion on who said it first, perhaps not Keynes or Churchill, but never mind.
I’ve been saying that there is no evidence of patients being diverted from seeing their GP through online help, and now that’s changed.
Our evidence is from two hard tests to see whether askmyGP can reduce demand. The first is to measure overall demand (by analysing all consultation records for practices in time series over months) and we’ve seen no measurable change up or down, a valuable finding in itself. Demand doesn’t increase even when 20% of it now arrives online. Nor have we seen overall reductions.
The second test is at the patient level, where we offer symptom specific NHS Choices information to patients. Many view this and find it helpful, but very few are deflected from consulting: we measure this continually, so far only 30 out of 38,000 episodes.
Then this Dutch study arrives, high quality evidence of 12% overall demand reduction. Enormously interesting, because the Dutch registered list and capitated system is similar to ours in the NHS (though insurance funded). The reduction was over 2 years and the result not only of the technology but also a complex intervention of GPs advising and encouraging their patients to use it.
But the technology matters too. It’s notable that while NHS Choices is also very popular, there is no evidence of demand reduction as achieved by thuisarts.nl. It was created by NHG, the Dutch equivalent of RCGP. The differences between the two websites may appear subtle, but the fact is, one of them works.
Our aim with askmyGP has always been to make it easier to manage demand, and it’s delivering. One practice manager told us this week, “can’t tell you how helpful the online system is”.
But reducing demand has been an aspiration, subject to finding something that works – perhaps we are now a little closer.
Some of you reading this may be in a position of power and influence. With these new facts, I know what I’d do.
Harry Longman
- Published in Evidence
Should patients be heard but not seen?
Dealing as I do with GPs week after week I admit to a twinge of envy that I will never personally be able to help a patient as a doctor, while they get the privilege every day.
But we get a little something from the feedback patients leave on askmyGP, and I wanted to share with you everything that’s come in the last 24 hours. Each one carries a story, and they are typical of recurring themes over the last two years.
They range from the simple, for which I’m grateful:
“Excellent facility.” male 54
to the more specific:
“Well structured questions to analyse symptoms etc.” male 62, sciatica
solving a real problem for many stressed parents:
“Much better as can use at any time and also don’t have 2 keep trying 2 get through on the phone in the morning” Parent of 3 year old, earache
and towards the other end of a lifespan, relief about the:
“Option for relatives of elderly patients.” on behalf of a 96 year old
Improving access without increasing surgery hours, and the importance of rapid response:
“This system worked well for us the first time we used it. We emailed out of hours but got a fast response as soon as the surgery opened.” male 81
Lastly something rather special, helping the clinical encounter itself by changing the channel:
“I get nervous talking about personal matters – this way the Dr can see what they are dealing with prior to speaking with me” female 44.
The desire to help one another runs deep in the human psyche, and I think that is why, above all the cacophony of crisis, the long term studies of job satisfaction always feature GPs near the top.
Don’t talk yourselves down, and don’t dwell on the latest “GP-as-victim” blog in the columns of Pulse. Margaret McCartney writes powerfully in this week’s BMJ on the intrinsic value of long term relationships which GPs enjoy with their patients, unique not only among the professions but specific to general practitioners.
Treasure it, enjoy it, guard it.
Very best,
Harry Longman
PS Many more have enquired since last week about how to get Resilience funding for their practice to improve service and workload. We are doing our best but it seems time is tight, so please get in touch soonest.
PPS I’m a big fan of Julian Patterson’s NHS Networks blog and this week’s consultation on STPs is a must. Light up a grey day!
- Published in Evidence
How does GP practice list size affect patient satisfaction?
This poster was presented at the European Forum for Primary Care annual conference, in Riga, Latvia, September 2016.
The data source is all English GP practices by list size, and the GPPES survey data for the same practices.
A clear relationship was found between the top score “Very good” and practice list size by band. Note that the critical distinction is between the score “Very good” and “Good”. The often used tactic of combining the top two scores makes the relationship disappear. However, given that 85% of respondents gave the top two, which is typical of surveys where most people are “nice” unless they have a particular complaint to make, I submit that the difference is useful.
- Published in Evidence
- 1
- 2