“Do you shop online?” Rural Ruskington GP moves 80% on day one
The staff room looks out over fields, a couple of hens pecking in the long grass over the fence. We’ve driven Lincolnshire’s challenging roads and arrived through quiet village streets and bungalows. Think everything Salford isn’t: elderly, stable, families and retired.
The new record set by Ruskington Medical Practice was to abolish the old and launch a completely new system from receipt of order in just ten days.
It’s the last place in the UK you’d expect to see this, but from day one they have got 80% of demand online.
They know that almost everyone under 65 has online access, and a large proportion of much older patients. The patients haven’t yet realised there’s an easier way to get help, so if they ignore the GP recorded message, the receptionist asks:
“Do you shop online?”
That simple question, almost always answered yes, means they can be directed to the website (or sent a welcome email) and off they go. Request arrives online, it’s sorted to the appropriate person, and completed within a median 91 minutes. Only 23% need a face to face or visit.
Credit to practice manager Jules for that phrase – we love simple. She’s happy, staff are happy, GPs happy, and patient feedback shows 78% say the new system is better (one aged 90), only 12 days in.
Jules tells me demand is below prediction, which I find slightly annoying as we do like to get this right.
I’ve counted and “Do you shop online?” has exactly half the syllables of “Patient Communication Strategy”. It would be funny if it wasn’t sad, but NHS England’s Patient Online programme has taken 8 years and spent countless £millions of taxpayers’ money on telling patients to book appointments online, and they’ve reached 4%.
It hasn’t worked and it will never work because GPs are smart enough to realise that allowing patients to book all their time will waste a good 2/3rds of it.
Here’s the offer that works for patients:
Tell us who you are and what is your problem, and we’ll work out how to help you. Boom.
You’d be amazed how many times GPs tell me “this wouldn’t work for our patients” – perhaps because they’ve tried something which didn’t work. That is why simplicity is so important, and why Computer Must Never Say No.
Ruskington at 80% still welcome those with no online access. Suburban Hounslow is another new launch, 86% online, Salford remain highest at 98%.
We’re looking forward to a Surrey commuter practice making the last launch of 2019 on 23rd December, and a Lincs seaside town the first of 2020 on 2nd January.
Never know who might set a new record…
Harry Longman
PS Often a fear of “opening the floodgates” leaves people torn about the risk of change. In the recorded webinar Understanding Demand we examine the evidence of what happens. Free to register.
For an idea of how the askmyGP could put you in control of your day, click here to get our four user stories.
- Published in Case studies
Digital First GP: Blackfriars Salford gets 97% online
The walk down from Manchester Piccadilly is a fascinating cityscape, and then crossing the river Irwell into Salford it seems everything is in flux.
Here, between the £180/night Lowry Hotel and the £35/night Salford Arms Hotel, lies Blackfriars Medical Practice. Perhaps that’s a metaphor for the patients Dr Babar Farooq and his team serve: young, mobile, diverse and with fortunes right across the spectrum.
It’s free to join his list and free to get help – the NHS is a great leveller.
What’s unique is that when Blackfriars launched askmyGP three weeks ago they moved 97% of their patient demand online, from day one.
There’s no messing about – Linda on reception simply tells the patients what they need to do. They send online, they get sorted within a few hours (median time to complete the episode is 193 minutes). Computer never says no.
Inside the practice with the phone not constantly ringing the drop in stress and pressure is palpable. They are bouncing. Babar keeps telling me how happy he is, and he’s resolving 38% of requests simply by message.
Patients? 86% say the new system is better. “I was surprised at how quick my question was responded to. Much faster than calling.” is a typical response, female 29.
Their demographic is young, mostly 20s and 30s, so we wouldn’t expect every practice to get this many online, 80% would be more reasonable for the average normal digital first GP.
Blackfriars in week 3? They’ve just ticked up to 99%.
Harry Longman
Pictured, between the yellow sign and the railway bridge, ground floor.
- Published in Case studies
Celebrating one million patient requests
One million patient milestone reached by online consultation and workflow system askmyGP
One million patient requests have been managed by GP practices using the askmyGP online consultation and workflow system since September 2018. The system is used by practices across the UK with a combined list size of 545,485. Clinicians at the practices use the system’s online triage tools to prioritise and deliver care by secure message, telephone, video or face-to-face appointment.
64% of patients chose to contact their GP online via the practice website, while the remaining patients phoned their practice. Half of patient requests were completed by the practice in two hours or less, including requests made online outside normal surgery hours.
Patients asked for face-to-face appointments in only 25% of cases. 45% of patients asked to be contacted by the practice by phone and 30% asked for a secure message from their clinician.
On reviewing patient requests, clinicians decided to see 37% of patients face-to-face. 88% of patients who needed an appointment attended the practice on the day they contacted the practice.
Across the one million patient requests, 6.5% of patients on the practice list made contact each week.
The one millionth patient request was received by the Concord Medical Centre in Bristol, which has been using askmyGP to manage all of its patient requests for more than two years. Senior partner Dr Simon Bradley said: “With askmyGP we are getting through the work more efficiently and continuity of care has improved too, with more patients consulting with their preferred GP. There are days where all outstanding consultations have been completed by 5.30pm, allowing the duty GP to manage urgent problems and process late requests that otherwise would have been passed forward to the following day.”
Harry Longman, chief executive of GP Access Ltd, the company behind askmyGP, said: “This is a major milestone and we are delighted that askmyGP has enabled a million patients to get help sooner from their own GP. That’s only possible by making it easier for practices to understand, predict and manage patient demand much more flexibly, putting them in control of who they see and when, managing their resources appropriately for each patient.”
- Published in Evidence
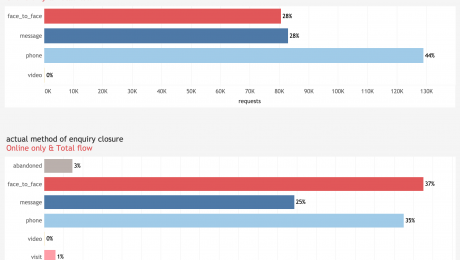
Patient preferences and clinicians’ choices in Q3 2019
The latest figures from askmyGP reporting patient contact preferences are consistent with those from earlier in the year. Data show continued low demand among patients for video consultations (0.06%).
When offered a choice of ways to talk to their GP, 27% of patients expressed a preference for a face-to-face appointment, 28% preferred to be contacted by secure message and 44% by phone. Slightly more patients asked for a face-to-face appointment than in previous months, but clinical decisions and actual method of delivery remain consistent.
The askmyGP data is drawn from practices with diverse patient populations receiving a total of 308,000 patient requests during the period. The data illustrates patient contact by clinical episode, with video consultation with the patient’s usual NHS GP offered at no extra cost to either the practice or the patient.
Clinical judgement always takes precedence, meaning in some cases simple queries might be addressed by a quick answer by phone or message, while more complex presentations will warrant a face-to-face appointment, even in cases where this has not been requested by the patient. Practices are not bound by their patients’ contact preferences, but they use the information to guide their responses to patients.
13 November 2019
- Published in Evidence
The dark side of digital inequality
If you’re a GP you will by now be familiar with the NHS England requirement for “25% of appointments to be bookable online”. If you’re a commissioner you may be fretting about how to measure it. Anyone else is most likely bemused by another arbitrary number of little relevance.
But there’s a dark side to arbitrary requirements, and with this one it is faced by the digitally disadvantaged. We instinctively know that those least capable of booking online, for reasons of age, deprivation, mental capacity or simply being ill, are disproportionalely most in need of help from their GP.
The good Dr Julian Tudor-Hart called it the “Inverse Care Law” and it can only be overcome by deliberate policy. By carving out GP capacity for a relatively advantaged group, this policy stokes and promotes that law. Shame.
You may look to BMA guidance on how to dance around the policy: in essence, 25% can be for any clinician, at any time, so it could be all the HCA appointments bookable 4 weeks hence. That ensures the box is ticked, but do we really want to manage compliance by frustrating policy?
Regular readers would expect me to offer a radical and practical alternative, and I’ll try not to disappoint.
We believe that 100% of patients should be able to get help online. And we believe that 100% of patients should be able to get help by telephone. Same goes for walk-ins.
How so? It’s all the same capacity, none is reserved for any group or mode of contact. The point is that a patient can’t reserve any GP capacity, it’s up to the GP to decide what is the best way to help. Patients can request help by any mode, but all requests go into the same flow at the same time, managed by the GP according to need: none has an advantage.
We are concerned to make life easier for both patients and GPs, and we know that online requests are much faster for GPs to deal with so we encourage patients to go online. It turns out that the 25% figure is unambitious. The lowest rate of online requests for any of our total flow practices is 35%, and the average 56%. I visited one in a perfectly ordinary part of Wigan last Wednesday which gets 75% online. That’s Wigan, not Westminster.
Median time to complete a requests at the practice, Shakespeare Surgery, is 31 minutes (if they need to be seen it will be later the same day).
In summary:
– patients will do what works for them, not what they are told
– online requests can work for all ages and conditions (though usage is lower with greater age)
– online is more efficient for GPs and receptionists, freeing up time for those who still need to use the telephone.
In order to deliver the outcomes we all want, system change not arbitrary targets are needed, and suddenly it makes sense to abolish the existing assumptions and methods.
We’ve added a criterion by which we judge progress with askmyGP:
The service must benefit non-users.
Harry Longman
- Published in Comment
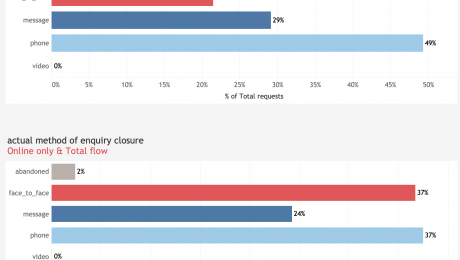
Latest figures continue to show low demand for GP video consultations
The latest figures from askmyGP reporting patient contact preferences show there has been no change in the low demand among patients for video consultations.
The askmyGP data for the second quarter of 2019 is drawn from practices with diverse patient populations receiving a total of 220,000 patient requests during the period. The data illustrates patient contact by clinical episode, with video consultation with the patient’s usual NHS GP offered at no extra cost to either the practice or the patient.
When offered a choice of ways to talk to their GP, 21% (Q1 25%) of patients expressed a preference for a face-to-face appointment, 29% (Q1 28%) preferred to be contacted by secure message and 49% (Q1 47%) by phone. Patients requested a video consultation in less than 0.1% (Q1 0.1%) of cases.
While practices are not bound by their patients’ contact preferences, they use the information to guide their responses to patients. Clinical judgement always takes precedence, meaning in some cases simple queries might be addressed by a quick answer by phone or message, while more complex presentations will warrant a face-to-face appointment, even in cases where this has not been requested by the patient.
13 August 2019
- Published in Evidence
Making it easier for patients (shock!)
“The patient journey…” We are fond of that phrase in the NHS, aren’t we?
That’s in the parallel universe of politics and pipedreams. The reality when we become patients is often very different. As one GP tweeted last week “Have to say being stuck in a trolley queue for over 3 hours got me thinking about patient flow”
At a practice on Wednesday a receptionist told me of the time she had a patient across the counter and had just explained they had no appointments left. He pulled out a pink screwdriver and started waving it at her. In that situation you would remember the colour of the screwdriver, though I was unable to see why a screwdriver would change the availability of appointments.
Wherever you enter the system, it can be deeply frustrating, when you know what you want and just can’t seem to get it. The patient journey we all want is one that works, and if it did, the NHS would be far cheaper to run.
We have a shockingly radical thought: “Make it easier for patients to get help”.
In general, most of us now start looking for local services online. That means the GP practice website is the very start, and what could be more important than getting this right?
Having looked at hundreds, they fall into three main groups:
1. Standard commercial offerings – low cost templates, everything included, ticks all the boxes.
2. Boutique designs – beautiful graphics, videos and moving images, where what you want must be somewhere…
3. Push-you popups – wherever you go on the site, they tell you what you want and it’s very hard to find a way around.
The problem we felt with all of them is that they don’t help the patient find and do what they want to do.
We don’t do websites, but we found someone in Tim Green at GPSurgery.net who does, and starts with patients. He tells me that most patients click on:
– how do I get an appointment?
– repeat prescriptions
– meet the team.
Aha. So that’s exactly what we put on the home page of our patient demo site Bramley Surgery.
Do try it, and we would love your feedback on the patient journey. Send in a request and we might even reply (sorry, no actual medical help).
Here’s the news: we have bundled one of Tim’s wonderful websites free with our Transform and Improve Pro packages. You can stay with your old site, but making it easier for your patients turns out to have a beneficial side-effect.
With 57% of demand now online, they make life much easier for you too.
Regards,
Harry Longman
- Published in Comment
Ben Gowland talks to Hugh Reeve
Delighted to share a surprise with you which I first heard on Wednesday.
Many of you will know Ben Gowland of Ockham Healthcare and his regular podcast.
This week he interviewed Dr Hugh Reeve of Nutwood Medical Practice in Grange-over-Sands, Cumbria. It’s 25 minutes of straight-talking on why they implemented askmyGP and what happened.
I’ve learned a lot from it too, about the importance of continuity for GPs as well as patients. As Hugh says, it pained him when patients had to wait days to speak to him, or were then passed around to others. Rework was bound to follow.
I love the bit where he says it’s not a bolt on, and where he says after 6 months each GP has shaped it for themselves. This is one of the most elderly populations in the UK, and they are now at 40% online. Quite a story.
Harry Longman
PS Do sign up to get Ben’s regular blogs.
Patient feedback:
- Published in Comment
New PM, new pledge on GP waits
How did you feel about the incoming prime minister’s pledge in his very first speech outside Downing St?
“My job is to make sure you don’t have to wait three weeks to see your GP”
Every PM I can remember from Blair to now Johnson has said as much, and what have they done?
– the 48 hour target
– the contract giveaway of 2004
– the Prime Minister’s Challenge Fund
– the Vanguards
– training 5,000 extra GPs
– the GP Forward View
– recruiting 2,000 foreign GPs
– the online consultation fund
I’ve probably missed a few, do fill in the gaps.
Every PM has watched waiting times increase and continuity of care fall. I’m picturing the ships they launched now a line of rotting hulks…
Nothing wrong with the ambition, what’s missing is method. METHOD, how, based on evidence, are they going to do it?
Practices we help measure their patient service in minutes not weeks, and with a choice of named GP, and in fewer GP hours. They’ve got there quickly and at low cost.
On Wednesday I met another practice in Lincolnshire for their Pathfinder diagnostic, they decided to go ahead on the spot and in three weeks time, they will prove it all over again.
We have found over the years that it’s best to ignore the fads, fashions (and indeed the funding streams), and pursue relentlessly what works.
Our approach doesn’t win friends in high places, so I’m not going to sit by the phone. Perhaps some of our happy GPs would get in touch with the PM, give him one less thing to worry about.
Harry Longman
- Published in Comment
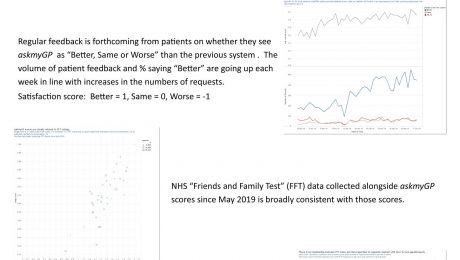
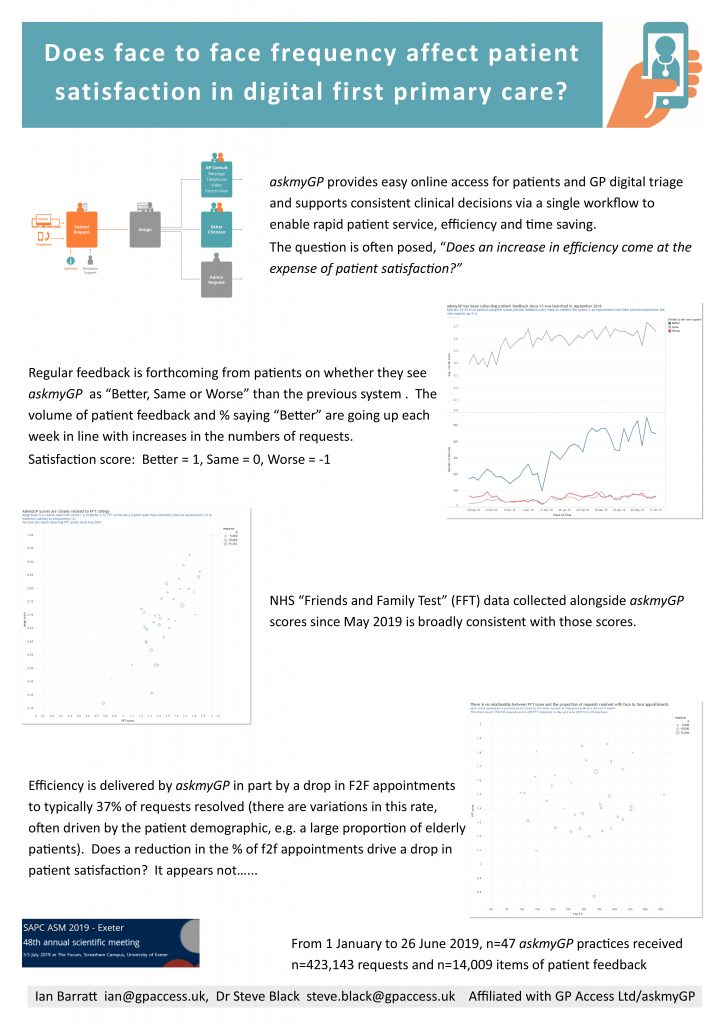
Does F2F frequency affect patient satisfaction in digital first primary care? SAPC Exeter ASM poster
Many have wondered whether patient satisfaction is affected by their chance of seeing a GP face to face. The study done for the Exeter Annual Scientific Meeting of SAPC (Society for Academic Primary Care) analysed 14,009 patient feedbacks from 423,143 episodes managed through askmyGP from 1 January to 26 June 2019.
Presented by Ian Barratt and Steve Black at the conference. Download pdf here.
- Published in Evidence