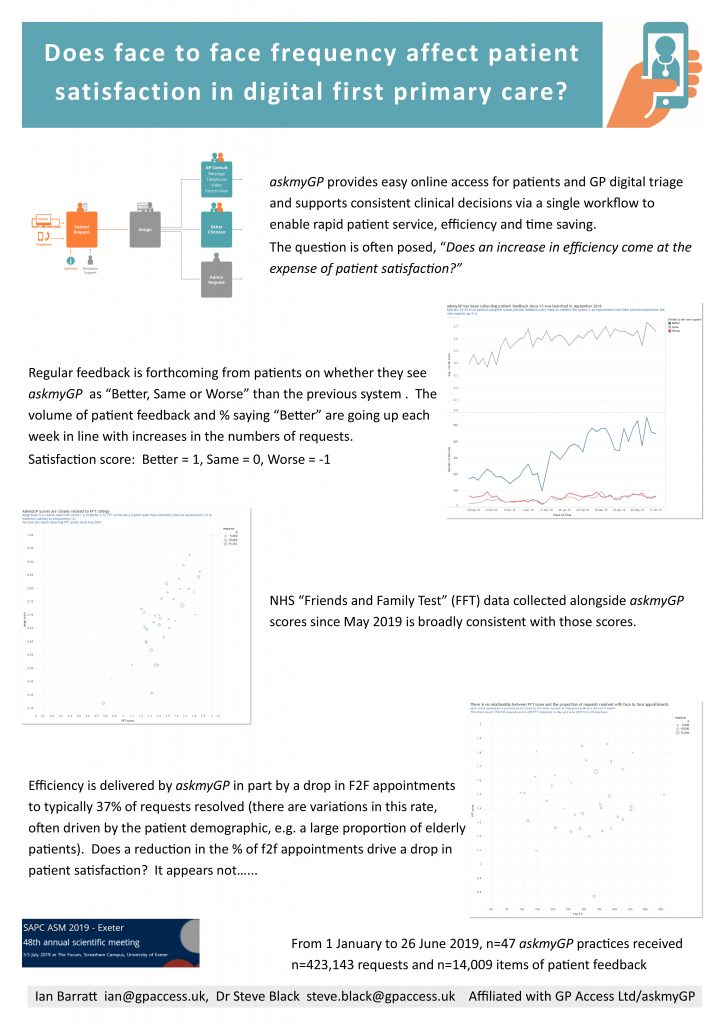
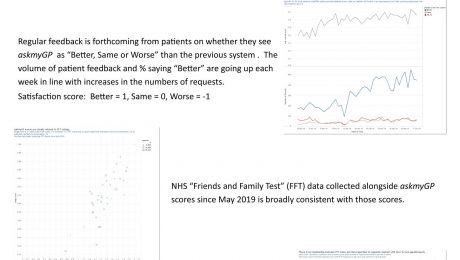
Does F2F frequency affect patient satisfaction in digital first primary care? SAPC Exeter ASM poster
Many have wondered whether patient satisfaction is affected by their chance of seeing a GP face to face. The study done for the Exeter Annual Scientific Meeting of SAPC (Society for Academic Primary Care) analysed 14,009 patient feedbacks from 423,143 episodes managed through askmyGP from 1 January to 26 June 2019.
Presented by Ian Barratt and Steve Black at the conference. Download pdf here.
- Published in Evidence
Shudder at NHS 111 digital’s first million
Read this NHS Digital press release and shudder: “NHS 111 online hits one million triages mark”
You will be very familiar with the quality output from NHS111 sent to GPs from the standard version, where a human reads a list of questions from a computer to a patient, and based on their answers tells the patient what the computer tells them to do. Data shows the disposition is 8% to ambulance with a further 7% advised to attend A&E.
That process has now been fully automated into NHS 111 Online, and the number advised to attend A&E has reached 24.7%. Yes, almost one in four patients seeking help “when it’s not an emergency” is told that after all it is an emergency.
Over many years we’ve run audits, n>200k, where GPs labelled just 0.4% or 1 in 250 consultations as emergency. So we can estimate the proportion of false positives in the NHS 111 online dispositions at around 98.4%.
As you would expect, I have tested the system myself, in the interests of science. During a break in the weather we managed a cycle club run this morning and after 53 miles I am shot to pieces, so I tried “aching legs”. Answering just 6 questions, all truthfully and all negatively, except that the aching was all over, sure enough I got the result in big red letters: “Phone 999 now for an ambulance”
Folks, if you read the press release they are actually proud of this. I put the figures to Simon Stevens at a Reform meeting last week. Earlier he had spoken of the benefits of machine learning in assessing images, an application which makes sense as computers are good at comparing similar things and looking for differences. When it came to 111 he assured the room that results would improve when the algorithms had more cases from which to learn. They’ve had a million, how many do they want?
247,000 innocent patients have been advised by this abominable software to call an ambulance or attend A&E. Tariffs vary but if we take an average of £200 (ambulances much more) that’s around £50m, almost all of it overtreatment. We are told that ambulances and hospitals are under pressure and want to reduce demand… is anyone in Skipton House paying attention?
Suppose these million patients had been diverted to a qualified human to assess their needs and respond appropriately, that £50m could have been invested in front-line services so beloved of politicians.
My only hope is that most patients had the good sense to ignore the advice. But what have we come to when the NHS is spending money to make people afraid?
We get asked to bid for contracts with CCGs to provide online consultations through the intriguingly named “Dynamic Purchasing System”. Most of the specifications require an algorithm to triage patients automatically to an appropriate disposition. We explain why we won’t do that because it would be both wasteful and dangerous. We don’t win any DPS contracts.
It doesn’t have to be like this. Public money could be spent on evidence based interventions. Ploughing our own evidence based furrow can be lonely but we’re going to keep on doing what works. As far as we know at 20,000 per week we’re already the largest provider of online consultations, mostly from practices self-funding because they make such a difference to their workload and profitability. They absolutely love it.
Cheer up, believe that better is possible, right now, and smile with the staff at Witley and Milford practice.
Harry Longman
PS Barry Sullman showed me the numbers from his CCG this week, Balaam St winter A&E attendances fell by 24% in his first year with askmyGP. That’s the power of human intelligence.
- Published in Comment
Would you allow patients to book online?
It seems pretty clear that the main plank of government policy towards patients is: let them book their GP appointments online.
The new contract says that 25% must be available online, and they are investing £6.3m in the NHS App with appointment booking the headline feature.
Yet we all know that anything which requires compulsion or bribery is probably a BAD IDEA. The badder it is, the bigger the bung. Good ideas have a life of their own and no government can stop them.
Online appointment booking has been a contractual item for years, and yet while everything travel, banking or retail is online, only about 4% of GP appointments have gone that way. The technology is there already – it’s the GPs who don’t want to release appointments for self booking.
They know that without reception as the intermediary, many will be taken by patients who don’t need them, reducing equity of access for those in greater need. They are even paying receptionists from their own profits to suffer all the stress of turning patients away, rather than put everything online and leave the phone off the hook.
Yet we know that when they trust the practice to give them the help they need, patients don’t even want appointments. We ask them how they would like to be contacted and were astonished to find the average at only 25% by face to face, some down at 11%, GPs begging them to come in.
“Super service thank you for implementing it. Much easier than an appointment” wrote a lady in Somerset today.
So we turn to the Pilot Evaluation of the NHS App. Credit for publishing this for comment within 3 months, but let’s look at the detail:
- 34 practices, given lots of on site support and training over 3 months to 21/12/18
- 3,192 patients used it
- 337 appointments booked, and 106 cancelled.
Now I’m “just saying”, as they say, but in the same period and with only 28 practices we had 100,000 patient submissions on askmyGP. No appointments were booked directly, but they all got help and about 30,000 had a face to face.
We’re coming up to eight years old as a company and I’ve found it necessary many times to do the opposite of the zeitgeist. There’s never any guidance on being counterintuitive and it’s very costly, but what keeps me going is that it works.
I was at a Leicester practice this week for their training and the enthusiasm they have is infectious. Next week a couple more launch in Sheffield and Glasgow. They are all paying for themselves, taking control of their own workload. It’s becoming unstoppable.
Two quick things to do now so as to see the difference:
1. Do the patient demo and get how easy it is, without being able to book an appointment at Bramley Demo Surgery.
2. See how easy it is to respond by signing up to the GP Demo, triage 50 real patient requests.
Summer is coming, don’t spend evenings in the practice.
Harry Longman
- Published in Comment
How will PCNs work for patients?
New financial year, new contract – the rush to put QOF to bed is replaced by the rush to absorb the new implications of Primary Care Networks.
“Who do we want in our gang?”
Or is it, “Will anyone pick me?”
Anxieties from the school playground resurface. I was never any good at ball sports.
Already there’s a deluge of advice from all kinds of bodies, leadership development offers, model contracts and so on. Some of it is bound to be contradictory given the scale of change and I have to say a July start seems, er, courageous. Then again delay to anticipated fundamental change seems to be in fashion, so we’ll see.
I have a different question: how will PCNs work, from a patient’s perspective? In simple terms, patient presents with a need, GP decides the need is best met with a shared network person or service. How are they assigned, how long will they wait, who owns the case?
For the PCN, more questions arise. How will they predict demand, by type and volume? How will they manage capacity and measure performance? How will they allocate resources fairly between members?
I would love to hear your views. Please drop me an email with a few lines, or comment on the blog. No promises, but we’ll try to help.
Harry Longman
PS It has been a pleasure to work with our highly talented videographers this week, at a simply astonishing practice. Very soon we’ll have the result, from prosperous Middle England. It’s just so hard to cut several hours down to 3 minutes.
Meanwhile the same team has made a short, just over a minute, from the other end of the spectrum in multi-ethnic East London. Before it goes out on social media your can sneak a look at Be More Barry. Just lovely to brighten up your weekend.
- Published in Comment
BJGP: Patient use of an online triage platform, evaluation of askmyGP v2
We’re delighted to inform you today of the open access publication from Abi Eccles et al:
“BJGP: Patient use of an online triage platform”
It’s the first independent study of askmyGP and it’s well worth reading in full. I will quote the conclusion briefly:
“Patterns-of-use and patient types were in line with typical contacts to GP practices. Though the age of users was broad, highest levels of use were from younger patients. The perceived advantages to using online triage, such as convenience and ease of use, are often context dependent.”
What comes through for me is the very ordinariness of the online demand. It’s the same as normal demand, same patients, same conditions, same frequency by day of week and time of day.
There’s more on patient feedback too, with themes extracted which are very familiar to us. We’ve quantified the age question in our study on “Age specific adoption of online consultations.”
What this study adds is online usage orders of magnitude greater than any previous paper, with 5447 patient episodes from 9 practices in 10 weeks. Data collection was May to July 2017, which was our previous version 2 platform. Since then the same principles have been carried forward to v3 with a new design and many more features. Growth in usage means that we are now collecting the same volume of data roughly every two days.
The scope for further research is increasing daily with an anonymised database of some 300,000 episodes, unique in general practice. If you’re an academic in the field, we welcome the opportunity to collaborate, particularly on studies of the GP practice as a whole, not just online components.
Benefits for patients and GPs are the product of system change.
Regards,
Harry Longman
PS See how patients interact with askmyGP on our Bramley Demo Practice.
To experience the GP side, start with our free online demo.
- Published in Evidence
The Tweety of Witley & Milford
It was a tweet from a regular GP partner (yes, they’re all special).
It was last Sunday lunchtime. Why then? For fun. For sharing. For sheer joy and pride in work. For having something to say.
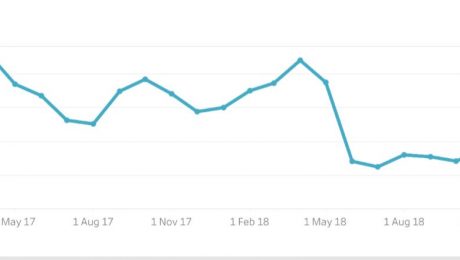
It had the image of a runchart, that simple device which is still the best way to show what happens to some characteristic over time, this one monthly from Feb 17 to Feb 19.
Now what’s remarkable about the characteristic is that it’s “Average days waiting to see GP”. That may seem obvious enough to a patient (oh yes, we’re all patients) but this was from a GP.
If you’ve noticed in all the medical press, Pulse, GP Online, BMJ, NHS England and so on they all harp endlessly about the pressures of workload, stress, burnout, early retirement of GPs and so on, but nairy a word about patients.
Now here’s a GP doing data about what matters to patients. How long to get help.
I can almost feel that defence welling up inside you “It’s not the only thing that matters to patients!”. Yes, we know it’s not the only thing, what also matters is the professional care they receive, and for many relational continuity with a named GP. But there’s no point in praising the wonderful professional care which patients can’t actually get.
Everyone knows the single biggest theme in the general media concerning GPs is the time waiting to get help, and in our own surveys of practice staff, the dominant theme is the difficulty in giving patients the help they need soon. Equally, the dominant theme by far in our patient feedback is gratitude for the speed of response.
Yet nobody is measuring the waiting time, what matters most to patients. Where are you NHS England, Scotland, Wales and NI?
We must turn to the story in the data. From Feb 17 to May 19 it starts with a range between 2 and 5 days wait, variable in such a way that stats geeks call “out of statistical control”. Others would say it’s all over the place.
Then it changes completely to a new mean of 1.5 days with random variation of +/- 0.3 days. This is in statistical control.
If you aren’t curious yet, there’s more. Discussion follows where the author Dr Dave Triska of Witley & Milford Surgery is asked what extra resources he needed to achieve this. “Mmmm we didn’t recruit anyone, in face we lost 6 sessions as we changed over due to retirement”
There’s no shortage of GPs here – they’ve saved a whole one.
What about personal care, stress? “It’s a pleasure most days to give people what they need – rarely overrun now even with 30mins with people dotted through the day”
So some patients are getting half an hour. And by the way, we know they achieve 91% continuity, choice of named GP.
People, this is history in the making, I don’t know how it will be looked on in the future but I’m calling it:
The Tweety of Witley & Milford 2019
Be the witnesses.
Harry Longman
This page is not for patients, who must find their own practice website to use askmyGP.
- Published in Comment
Cheer up
NHS commentators specialise in gloom as I don’t need to remind you, and this week they have had plenty to moan about with the publication of the latest Nuffield/Kings Fund British Social Attitudes Survey.
Overall satisfaction with the NHS is down 3%, and for the fourth year running the principal reason cited, at 53%, is “It takes too long to get a GP or hospital appointment.”
As sad as it is predictable, the only response from all parties has been “Give us more, more money, time, resources, GPs”. It’s not happening, GP numbers have shrunk this year.
Our latest practice launch this week was a middle of the road performer, with about 60% of demand “on the day” and a long spread thereafter leading to an average wait of 5 days.
In week one they dealt with almost all demand on the same day, achieving a median completion time (that’s completed, not just first response) of 49 minutes. Patients have loved it, with 8 to 1 saying it’s better. All done with no more resources – it’s only possible by saving time, managing 2/3 remotely.
I’ve had two contrasting conversations with practices this week. One is in a prosperous market town, in a brand new multi £million health centre. The GPs know they are making patients wait four weeks for a “routine” appointment, and they are quite happy with that, protected by their contract and local monopoly.
We can’t help them.
Imagine any normal company like us treating our customers like that – we’d be out of business in a minute. And that is why Babylon GP at Hand has a point, even if we don’t share their business model.
The other practice is in a decades old building, serving one of the poorest populations in their city, a minority having English as a first language, and dealing with huge problems of deprivation. Yet they have an absolute passion to help their patients, already providing a superb same day personal service. They just want to make their own working lives sustainable too.
We can help them.
Looking forward to more launches next week. Glad to say that every one gets easier with new features, this week it’s the NHS Spine lookup for patients, improving accuracy and saving time on reception.
Regards
Harry Longman
PS GPs with that service ethos, don’t miss out any longer. Start with our free online demo.
- Published in Comment
Our response to DHSC Code of Conduct
The Department of Health and Social Care published on 19/2/2019 its Code of Conduct for data-driven health and care technology.
Our response to the ten principles follows:
- Understand users, their needs and the context. askmyGP users are broadly two groups, patients and providers which includes all GP practice staff. Our design principles are for simplicity and ease of use, a difficult task when appealing to patients of all ages and abilities, both in general education and familiarity with online tools. We cater equally for proxies (parents and carers), all gender expressions, and keep language simple to help those with limited English. To assess our effectiveness we monitor age specific adoption by patients in each practice, and feedback from patients informs our development process.
- Define the outcome and how the technology will contribute to it. Our mission is to make it easier for patients to get help from their own GP, and easier for GPs to provide that help. We measure attainment against this outcome by volumes, response and completion times, and measures of efficiency through resolution mode by providers. We also collect and monitor patient feedback and present all measures to the provider organisations.
- Use data that is in line with appropriate guidelines for the purpose for which it is being used. We comply with all relevant legislation including GDPR, Data Protection Act 2018 and collect data only for necessary purposes. Personal data is processed on behalf of providers (the data controllers), stored and transmitted encrypted and over the secure N3/HSCN network. Anonymous data may be used for research and marketing purposes as allowed under the same principles.
- Be fair, transparent and accountable about what data is being used. All data is used in accordance with Caldicott principles, and the conditions are agreed by patients and providers.
- Make use of open standards. We support the use of open standards and wherever technically possible provide open links to others for legitimate interoperability reasons. We use standard NHS number coding for any authorised data transfers.
- Be transparent about the limitations of the data used and algorithms deployed. We collect and transmit plain text and other file formats between patients and providers, but we do not use algorithms to produce triage decisions or advice to patients.
- Show what type of algorithm is being developed or deployed, the ethical examination of how the data is used, how its performance will be validated and how it will be integrated into health and care provision. We do not develop algorithms. We do offer a third party service with Isabel Healthcare, which uses a machine learning approach. Our users may enter any number of symptoms, and be shown a range of possible conditions.
- Generate evidence of effectiveness for the intended use and value for money. Integral to our offer to all customers is standard reporting on usage, patient service, timeliness and efficiency through the use of askmyGP. We provide an economic model (Loadmaster), configurable by each customer, which demonstrates their value for money. We also conduct our own analysis of performance and value and may publish on this site and in other media from time to time.
- Make security integral to the design. From the outset of design, security has been built into askmyGP. Key features include:
- N3/HSCN access required for all live patient data by providers.
- Encryption of all patient data in transit and at rest
- Strength checked passwords required for all users.
- Separate code and database for live and demo systems
- Independent penetration testing and fulfillment of all comments raised.
- Define the commercial strategy. Our strategy is that self-funding customers should see a high rate of return from their investment, and do so from the date of launch (typically four weeks from engagement). Growth is therefore not dependent on taxpayer funding, but on efficiency and financial savings generated through the use of our services.
Harry Longman, 21 February 2019
- Published in News






New PM, new pledge on GP waits
How did you feel about the incoming prime minister’s pledge in his very first speech outside Downing St?
“My job is to make sure you don’t have to wait three weeks to see your GP”
Every PM I can remember from Blair to now Johnson has said as much, and what have they done?
– the 48 hour target
– the contract giveaway of 2004
– the Prime Minister’s Challenge Fund
– the Vanguards
– training 5,000 extra GPs
– the GP Forward View
– recruiting 2,000 foreign GPs
– the online consultation fund
I’ve probably missed a few, do fill in the gaps.
Every PM has watched waiting times increase and continuity of care fall. I’m picturing the ships they launched now a line of rotting hulks…
Nothing wrong with the ambition, what’s missing is method. METHOD, how, based on evidence, are they going to do it?
Practices we help measure their patient service in minutes not weeks, and with a choice of named GP, and in fewer GP hours. They’ve got there quickly and at low cost.
On Wednesday I met another practice in Lincolnshire for their Pathfinder diagnostic, they decided to go ahead on the spot and in three weeks time, they will prove it all over again.
We have found over the years that it’s best to ignore the fads, fashions (and indeed the funding streams), and pursue relentlessly what works.
Our approach doesn’t win friends in high places, so I’m not going to sit by the phone. Perhaps some of our happy GPs would get in touch with the PM, give him one less thing to worry about.
Harry Longman