Are you seeing higher than usual demand?
GP media is full of headlines to the effect that demand in general practice has been overwhelming in recent weeks. Our data from practices shows around 10% increase since January, peaking in March. Seasonal effects are normal, but is overlaid with the unpredictability of the pandemic (last year saw demand reduced 30%). There are real world reasons why demand is now high: secondary care waits, mental health issues and increased complexity. How can askmyGP practices adapt?
We don’t have a silver bullet but can offer some thoughts. Firstly, a couple to avoid:
– It may be tempting to delay non-urgent patients. This doesn’t really save work, as the patients still need to be dealt with and are more likely to chase, increasing stress.
– Shutting off online access when a number has been reached means patients will turn to the phone, increasing workload on the day, but they may lose trust in the online system longer term, increasing your workload.
We suggest continuing the tactics you would normally use, with these aims:
- respond rapidly to avoid patients chasing and rework
- encourage online access as it gives you the option to message patients
- manage the flow same day to keep you feeling in control.
1. Check the data that you have on demand, from your reports section. Trends over time will give you the longest view, while weekly demand shows the split by day of week. From the superuser menu Settings>Capacity planning helps with a simple way to estimate demand, as a % of your list size by week and by day. By default set to 6.5% of list per week for clinical and 1% admin, you can adjust these figures and save to dashboard. Some practices drive more demand eg repeat prescriptions through askmyGP, so it’s best to use your own figures.
2. Adjust rotas? Where possible, both timing and capacity (number of requests per session) will help. You’ll see on the dashboard how close total capacity comes to predicted demand, which is a good predictor of how well each day is going to work.
3. Adjust opening hours? Views differ on how best to organise. Many practices accept requests 24/7, responding only in core hours, and we’ve found that patients appreciate the convenience but rarely abuse the system. OOH requests are about 20% of the total, much of it just before opening time, and weekends are very low. Others don’t accept requests OOH or stop receiving requests some time in the afternoon.
Our evidence shows that this has very little effect on total demand (patients have to wait), but if the cutoff is too early, say before 4pm, it does drive demand onto phones which increases practice workload. Requests judged urgent should still be put onto askmyGP so the workflow is consistent and you have a true picture of total demand, while losing the ability to message patients.
4. Change service message? Any service message can be set at Settings>System to advise patients although we don’t know how well read they are. A short message is always better than a long one which is much more likely to be skimmed or ignored.
5. Assign new requests quickly especially at peak times. If there is likely to be a delay compared with normal service, you can send a preset message from the assign screen (“skip” bottom right, then the message dialogue appears)
They say that after rain comes the sunshine and we expect the normal pattern to be re-established before long. Roll on summertime!
- Published in Comment
What’s happening to GP demand?
Not for the first time in living memory, the GP media is full of headlines on demand taking practices to “breaking point”. It seems to me important that we bring the best data we can to bear on this question. It’s only good scientific discipline to diagnose the problem before attempting to apply a cure.
There are real world issues which could be driving some level of increased demand. Patients may have saved up issues during the pandemic for which now they want help. Long waiting lists for secondary care may increase the primary care burden. Concerns about covid, and long covid, may be part of the load. Complexity may have risen, with mental health issues more common. While all these are possible, I’ve seen no data to quantify the effects and we don’t know the detail of patient requests.
We can say that overall patient demand is at a new peak, compared with winter 2019 pre-pandemic, numbers up by around 5%. At this time of year demand usually flattens by a few % with spring weather so the relative change may be slightly higher. There is a much bigger change compared with April 2020, because demand fell by around 30% during the first lockdown.
How to measure?
While headlines can be made by choosing a suitable baseline, I think it’s vital to use consistent measures. Even though they are imperfect, the same measure year after year gives us a much clearer view than introducing different measures, imperfect in new ways. This is a key reason why we start from patient demand, driven by patients from outside the system it’s less subject to internal system changes.
How could system changes contribute to the headlines on demand? There’s public speculation that making access easier, particularly online access, could increase demand. No one can say that it’s never true, but pre-pandemic we found that overall clinical demand stayed predictable and constant around 6.5% of patient list per week, and was not affected by faster service. It is true that if supply was previously constrained then the true level of demand would become apparent, but this is not strictly new or increased demand.
English practices are being asked to provide new data, relating to appointments. Changing the measure to “activity” may seem a fine point, but if one patient request generates two activities (eg telephone call plus separate face to face) the activity appears to double, cf one pre-booked appointment. This could be misinterpreted as demand and on a large scale, very misleading numbers will follow.
So what to do?
There are calls to go back to the time before. I can understand that, at a human level we are acutely aware of loss of good times remembered. But thinking back, there were huge stresses, and patients who’d waited weeks to see the GP were suffering. Another form of double counting was the “just in case demand” – patients booking ahead speculatively, knowing that it’s hard to get an appointment.
Now there are calls to limit online access. We’ve always believed that practices should have control over their access channels, so they can programme times to accept new requests into askmyGP. The data shows that turning off out of hours has little effect on overall demand, and is only fair within the GMS contract, although we do have practices who accept requests at all times (and respond in hours).
However, if access is turned off too early, or after a fixed count is reached, unintended effects can follow. Once patients lose faith in the online channel being available, they return to the phone, taking up reception time in answering and more GP time as a phone call is needed in return, and the beauty of asynchronous messaging is lost. A downwards spiral results, where online demand falls, workload increases and waiting times increase, as does stress for all parties. Access becomes a lottery, and the very thing we want to avoid, digital inequity, returns. Those advocating the blunt instrument of limiting supply have not come up with a way to make it fair or based on clinical need.
Don’t give up!
Primary care has made huge and positive changes through the pandemic and we must not lose sight of the gains. I’m hearing of lengthening waits even for a phone call, queues of online forms awaiting triage, and many practices with very little incoming online or a token bolt on tool.
It has been striking to see askmyGP data show the proportion of requests resolved same day stay close to 83%, with half under four hours, even as demand has increased and face to face has ticked up to 10%. We’ve never said it’s easy, never said we’ve reached the destination, and our users are feeling the same real world pressures as all GPs. But I think we’re on the right track:
- online access for the large majority who can use it,
- digital triage in one click,
- a rapid, appropriate clinical response.
When times are hard, we can celebrate having in the UK one of the least worst primary care systems in the world. Given the ups and downs, let’s go forward rather than back.
“So much better service this is definitely the way forward thankyou.” Lincolnshire patient 8 minutes ago.
Harry Longman
- Published in Comment
Triage – do we need a new word?
We’re enjoying the sunshine, working a lot from home, and asking, how much has changed in primary care in a year, and how much hasn’t?
It seems quite a lot, as this sounds at face value rather like what we’ve been saying for ten years or so. NHS England planning guidance assumes that “total triage” should be embedded, and they mean permanently. Ah, but in the previous paragraph, they want 50 million more GP appointments! Well, that’s still based on supply led thinking, and I would so love to see a change of perspective, beginning with understanding demand.
Demand led thinking starts with the patient request, infinitely variable in every detail but conforming to quite predictable patterns both of timing and content. When access is constrained, it can be difficult to measure demand (because patients can’t get through), but trying to manage slots risks the wrong kind of supply and the wrong timing.
Unfortunately recent efforts to measure supply, requiring the generation of appointments, have served to exacerbate the problem by focussing minds on the numbers. “What gets rewarded, appears to get done. What gets punished, appears not to get done.” Human nature hasn’t changed, I think we can be pretty sure of that.
Yet the “total triage” tag has generated opposition, Helen Salisbury asking in BMJ “Triage is for emergencies. Can we start planning for a time when it’s no longer necessary?”
The origins of triage lie in war and emergency, from the French trier, to sort or select, and so “routine triage” may sound like an oxymoron. Before looking for a different word, it’s worth considering what is intended and what is the alternative.
The point of primary care is to cope with undifferentiated demand, and the NHS promise is for patients to have universal and free access. So long as they provide that access to their patients, GMS gives GPs full professional discretion as to how they do so. Reality bites because there will never come a time when there is sufficient capacity to give every patient exactly what they want, when they want, with whom they want and in the way they want.
As we’ve seen time after time, if patients have completely unlimited access to book a face to face consultation, while many use it well, some abuse it, but the problem is that you can’t know in advance who they are. More often, it’s not deliberate abuse but simply not knowing what’s needed, or from which clinician. Human nature again plays a part, scarcity ramping up demand. If it’s a long wait to get an appointment, I’d better book early “just in case”, and while medical need is unchanged, demand appears to rise.
That alternative reality inevitably means that patients must queue for as long as it takes, and we well remember the four, five and six week waits for appointments. I’m glad to say that particular noise has much abated this year, and however it is labelled, it’s thanks to GPs changing how they work. Still, it’s worrying to hear now of some patients waiting two weeks for a telephone call, which could still be called triage but is firmly based in a supply led system.
I suspect that much of the opposition to triage is that it is seen as a bolt-on rather than thinking and system change, which then means a gruelling experience of the process. Zoom fatigue, or telephone fatigue, is a reality. We need variety in the day, and we need human contact. Equally, wading through lengthy questionnaire forms is tiring on the brain both for patient and GP, where with too much information the first task is to sort the wheat from the chaff.
Returning to the goal of the system, we want to meet the patient’s need, in the most efficient way for the GP. Starting the process online is the best way we know for the vast majority of people, as in other spheres of life. We’ve found trusting the patients to use their own words in askmyGP has three key advantages:
– it’s simple and the computer never says no, so typically 70 – 80% of all patients will use it online.
– it’s fast to assign to the right clinician
– the GP has sufficient information to know the best approach, even if that needs a change later on. Time is only committed appropriate to need.
It’s never easy to change language and I don’t know whether “sort” is an improvement on “triage”, which at least has a medical association. Perhaps we should settle for describing the alternative as “unsorted”. I don’t think anyone wants to return to the waste of precious time seeing the wrong patients while the right patients were hanging on the phone trying to get through. GPs tell me a year since making the change, it came at exactly the right time and we’re never going back.
Harry Longman
Photo: Otis Historical Archives Nat’l Museum of Health & Medicine
- Published in Comment
Remote GP care and inequality – dispelling the myths
Calls for a review into how patients access their GP, and the potential barriers to them doing so, have highlighted the difficult decisions some practices are facing over remote consultations. The focus on video consultations, as opposed to remote or total triage systems, is based on concerns about equity.
Healthwatch England called for the formal review after its new report revealed the rapid switch from face to face to remote consultations in the last year has not met everyone’s needs. It found some patients are struggling to get through to their GP surgery, while other concerns include possible missed diagnoses, difficulties for people who don’t have access to the internet and for anyone whose first language isn’t English.
The NHS Long Term Plan stipulated that remote consultations (telephone or video) should be offered to all patients by 2021 but early take up was slow and the Covid-19 pandemic has been the catalyst for change. However the sudden necessity for remote consultation has revealed much about the preferences of many patients.
While an RCGP survey in July 2020, reported that more than 88% of UK practices were now equipped for online or video consultations compared with just 5% pre-pandemic, a King’s Fund report into digital access to GPs during the pandemic highlighted research which found that some of the initial enthusiasm for online access is beginning to wane.
Providing choice over method of consultation is vital
To ensure that gains made during the pandemic with regard to remote consultations are not gradually eroded, patients must be able to access services in a variety of ways. Making sure patients have access to online or video consultations is just the start.
Choice about the type of consultation and the ability to provide remote access to a GP (whether online or by telephone) is key. The Healthwatch England report found that, out of 1,190 people polled who had booked an appointment since March 2020, 75% had booked via telephone, 18% over the internet and 5% in person.
All too often video consultations are seen as a proxy for remote access to a GP, but not everyone wants or is comfortable with this way of communicating. However, there are several different online systems that can provide options to suit the patient. For instance, askmyGP provides a unique total triage platform for patients to access their GP in whichever way they choose. Offering an online booking service to those who are comfortable using it can relieve the pressure on phone lines, particularly at peak times.
We regularly review data from our system which is used by over 2 million patients to access their GP practice. This data tells us that several myths about remote access simply do not stand up to inspection. Here are just a few we have looked at:
“Patients prefer face-to-face consultations”
A typical GP practice sees about 5-8% of its list size each week and askmyGP is often handling that entire volume. 73% are going online to make requests and 27% are phoning the practice. With more people going online to make an appointment request, this relieves pressure on the phone lines for those who prefer to call. For our GP practices only 6% of patients requested a face-to-face consultation which shows that patients are happy to go online or use the telephone to access their GP.
“Older people are not internet savvy”
Older people make up a significant cohort of the patients using askmyGP to access their practice, still 50% at 70-75. However, for anyone less confident in using online services or who cannot access them, our triaging system ensures choice. Patients can still call the surgery and the receptionist can key in their information and arrange their appointment instead, it doesn’t have to be all or nothing.
“Remote access is unsafe”
Using askmyGP, practices can respond to requests appropriate to the patient need, rather than limited by supply slots. The BMA has also highlighted that the speed and convenience of access to GP services has improved for many as a result.
So, it is clear from our data that patients are happy with remote access, mostly by telephone or message, but providing choice over how appointments are accessed is key. An efficient triaging system can provide that choice and ensure that everyone is able to access the services in the way that is the best and safest for them.
Click here for more on how we can help.
- Published in Comment
Putting two and two together on GP workload
Like many of you I’ve joined in the clap for key workers on Thursday evenings, and very well deserved it is too. There’s little doubt in the public mind that the NHS has performed better in the pandemic than the government overall.
But working in the health sector we have every reason to feel not just pride but relief, as we are in relatively secure jobs while we see others all around lose their livelihoods in everything from hairdressing to aerospace.
This week another survey comes out from the BMA, GPs bemoaning their lot for one reason or another. In the eleven years I’ve been working with GPs, something like this appears almost weekly, predicting the end of the profession as we know it. Yet the GPs we work with are more secure than ever, loving the job and have never been better off.
Adding to the conundrum is disturbing data on numbers. As reported in GP Online, GP ftes are down 712 in the year to March 2020, and GP partners down 1,023. Yet in the same issue, GP locums bemoan the sudden loss of work in the pandemic, 81% seeing a drop in income.
I’m sure that, like me, you have many friends and relations in the medical profession and I’m sure that considered overall you wouldn’t disagree with what one observed to me, “We’ve never worked less hard since we left medical school.”
It’s amplified by leaders saying “We’re not going back to the working life we faced before the pandemic”.
I can’t wait to be rid of the restrictions on all our lives, but there’s little doubt that general practice will not return to the working format pre-covid. RCGP reported that face to face had dropped to 25% of consults, which seems high to me as our practices dropped from 30% to 2%. It has now crept back to 5%, while total demand is nudging up towards pre-covid levels.
Having discovered the efficiency of telephone triage overnight, partners will not offer face to face to everyone again, rehire all the locums and take the hit on their profits. We’ve been saying this for ten years, a few pioneers have said so for twenty years. Our latest askmyGP data, live here, shows 37% of requests are now resolved by message alone, no need even to telephone and much more time saved, while patient feedback is up too.
Practice after practice is discovering the same, but they all seem to go through a ritual of catastrophisation before they launch. At one this week the GPs were very adamant that Friday would be the busiest day, and I said they would remain very adamant until Friday. It came in with less than half even my predicted volume.
Another due to launch next week did the staff survey, and the biggest fear of the partners was higher workload. The biggest fear of all the other staff was losing their jobs because of lower workload. It’s a GP thing, and it goes with the territory.
With the huge extra resources now going into Primary Care Networks, I foresee very good times ahead for GP partners. If you’re a locum or salaried, apply as soon as you see a good opportunity. If that translates into better patient service, better quality and continuity of care, and more fulfilled professional lives, we all win.
So I’m very optimistic, but honestly, I’m bored with lockdown. I haven’t quite reached the point of sorting out my sock drawer, but I’m close, and that’s serious. Okay okay, “There’s never been a better time to sort out my sock drawer.”
Harry Longman
- Published in Comment
How will your PCN manage workflow, demand and capacity?
With the passing tomorrow of the deadline to sign up to the Primary Care Network DES a Rubicon will have been crossed for PCNs. The rehearsals are over, real money and commitments are at stake. But I want to know, how will they work?
A funding model is in place, a set of PCN duties and payments is agreed, no doubt controversially for some but that’s how it is. A list of professions is now 100% funded by the delightfully named Additional Roles Reimbursement Scheme.
But still I ask, how will they work?
Everything we do in the NHS needs to relate to its purpose which, however it is worded, amounts to helping patients overcome or manage their various medical needs and diseases.
The additional roles must be to help patients, who have needs. Which patients, what needs, when, with what measurable outcomes?
Forgive me if I’ve missed something, but the debates on funding, roles, governance and so on seem to be very far removed from these practical questions.
Consider the patient journey: present to GP practice, GP considers they would benefit from referral to a PCN employed clinician, say a pharmacist. How easily do they refer them? How soon can the patient be seen? How does the pharmacist manage demand from multiple practices? What is the right capacity for each kind of role?
A PCN I spoke to had a pharmacist one day per week in each of the five member practices. Neat, being five, but others will have 3, 4 or 7, and all different sizes. One may be mostly students, another elderly and with very different needs. What if our patient gets referred on Tuesday, just missing the pharmacist who calls at her practice on Mondays? And work or family commitments mean Monday never suits her?
Managing the workflow, demand and capacity for shared roles could be orders of magnitude more difficult than the same within practices.
I would love to know your thoughts on how, or ideas from your PCN. Yes, we are going to try and make it easier so you can make the most of the new resources, do let us know what you would like and watch this space.
Harry Longman
PS Last week’s blog looked at return on investment in askmyGP. David Evans replied to me that following their £35k investment in year one, they were saving £100k pa in locum costs. Not bad, indeed typical. Sujit Vasanth commented online “I can honestly say the change to askmyGP has been the most important (and positive) change in our practice in the last 10 years.” Thank you!
A number asked about spreading payments and I’m pleased to announce that we have responded with just that, it’s on the bottom of our Transform Express and it is now standard.
- Published in Comment
Why some of the best things are not free
Today I want to talk about a problem for us and for GP partners. We’ve always supported the GP partnership model as the most effective (while not the only) way to deliver high quality primary care, locally and with long term relational continuity.
Forgive me if you’re not a GP partner, no need to read on, but if you are I hope we can share some of your thinking as we are a small business with a turnover similar to a medium sized partnership. We value our independence and we want to help you use yours.
Throughout England GPs are able to access one of several suppliers free which enable them to comply with the edict to offer online and video consultations. We chose not to participate in this tender, as the allocation is random by CCG, no evidence of outcomes was required to participate and therefore it is impossible for GP partners to make an informed choice of supplier.
Not only are we competing with free, bluntly our service is around three times the price of others over 3 years. It’s a job to explain to people that it’s very different from bolt-on technology, as askmyGP enables system change like no other. We are not competing with point solutions.
This means that in addition to helping you comply with regulations, we need to sell on the concepts of “value for money” and “return on investment”. It has to be worth it for GPs making decisions as owners, those with skin in the game (I loved the wonderfully provocative book of that title by NN Taleb).
In the whole UK just four CCGs and one Welsh health board are fully funding askmyGP for all their practices, and they are flying, but let us face facts: the rest of you are going to have to pay directly. Which puts you in exactly the same position as thousands of other businesses, including ours, where investment is a decision you make to save time and money, improve your life and increase profits.
Now here is the good news: our customers are our greatest fans, and we are very grateful to them for their public support. Some recently set up a facebook group (I’ve applied to join). They are all over Twitter – last week @simondevial wrote “We’ve been using it for 8 weeks. In 28 years no other change delivered “what it says on the tin” like this.”
I was talking to Barry Sullman on Friday. He’s happier than ever after 2 years. “Using askmyGP has given my practice extra resilience, allowing us to easily cope with clinical staff shortages due to Covid, and sustain a high level of care dealing with every clinical patient the same day” He goes on to add “Last year was our best QOF year because of askmyGP. We were able to identify long term condition patients at the triage state and bring them in for care of their long term condition as well as the problem being triaged. As a result last year I reached virtually all my QOF targets before New Year’s Day!”
We hear lots like this. As a result we’re seeing the highest ever rate of enquiries from GPs, many of them unhappy with the free software imposed by their CCG with no consultation and no evidence.
However, many get stuck at the point where they need to pay, and when they are used to having everything for free, it seems odd. Yet the same people wouldn’t think twice about buying a holiday (a cost) or replacing the car (a wasting asset).
Last week my bank wrote to tell me the interest on my savings account is 0.01%. Compared with keeping £1000 under the mattress for a whole year, that’s just 10p extra, and they are threatening to charge us for looking after it soon.
I’m happy to report that increasingly partnerships are realising the very high rates of return they will make with askmyGP and deciding to invest, based on evidence, putting themselves in control of their destiny. Our practices managed 98,050 requests last week, 96% of them remotely, 69% of them received from patients online.
It’s not only the savings on locums (you will have noticed that locums are struggling to find work at present), so many echo @catiebagel’s tweet “Hope we can continue to deliver remote assessment and treatment where possible & if clinically appropriate. Often more convenient for patients and less travel has co-benefits for the environment. Agree, am so glad we had @askmygp in place before COVID hit. #greenergp”
You may have enquired with us a day, a week or a year ago. If you’re not convinced of the evidence, crawl all over our website, study our live data, ask your friends who are customers and look for independent views. If you don’t understand it yet, spend an hour on the webinar “How, but first Why, askmyGP works”.
If you’ve seen and heard enough, and you don’t want to waste a year on something free but with tiny usage and no savings, then now is the time to act for three simple reasons:
- the barriers to change have disappeared
- current workload is lower than ever
- money has never been cheaper
So many practices have got this far and then decided to hang on for taxpayer funding. They are still hanging on, six months, a year, two years later. Don’t be another disappointed hanger-on, be another delighted user, within a week. We’ve now launched close to 3% of UK practices – that’s enough to start a revolution.
Kind regards
Harry Longman
- Published in Comment
For the few, not the many
After peeling 3.5kg of potatoes in just ten minutes for Burns Night, I’m grateful again to Sam Farber, creator of the OXO Good Grips peeler. Motto “Make everyday living easier.”
His wife Betsey had arthritic hands and he saw how hard it was for her to hold a peeler. The new model came after hundreds of design ideas and iterations, but despite being four times the price of its bent metal predecessor, it’s now the choice of millions of able bodied sous-chefs around the world. I would never use anything else.
What’s the connection?
My time with patients on launch day in Hyson Green, Nottingham on Thursday was fascinating. Dozens of languages are spoken among this deprived population, making it one of the most challenging places in the country to deliver high quality primary care. I submit that this is the NHS at its humane best, universal and free at the point of care for the patient in need, whether from UK, EU or anywhere else.
I watched as a Polish man created his login to make a request on behalf of his girlfriend, trying not to “help”, rather to see where there might be the slightest trip or friction. His smartphone is set to translate, but the translate bar covers one of the text windows. He needs to click “Please accept the end user licence agreement” but his fingers are fat and he misses the small checkbox. Why not have a bigger box and shorter text, “Accept the terms”?
Next I sat with a Romanian interpreter, the lady next to her not the patient but her sister, working out how to send a request by proxy, then to be able to arrange a face to face with the interpreter present.
Patient situations are endlessly complex, and we must learn how to do better for all.
It is so much harder to build something simple than something awkward to use, and it is these extreme but everyday situations that drive us continually to fine tune the patient experience.
We’d had the usual comments from the staff that askmyGP would not work for all their patients (most practices tell us why their patients are different and won’t use it). In the event 69% of requests arrived online in week one, higher than our median 63%, and the feedback has been 100% positive.
I hope the title makes sense. Design “for the few, not the many” means everyone’s life is easier.
Harry Longman
- Published in Comment
The dark side of digital inequality
If you’re a GP you will by now be familiar with the NHS England requirement for “25% of appointments to be bookable online”. If you’re a commissioner you may be fretting about how to measure it. Anyone else is most likely bemused by another arbitrary number of little relevance.
But there’s a dark side to arbitrary requirements, and with this one it is faced by the digitally disadvantaged. We instinctively know that those least capable of booking online, for reasons of age, deprivation, mental capacity or simply being ill, are disproportionalely most in need of help from their GP.
The good Dr Julian Tudor-Hart called it the “Inverse Care Law” and it can only be overcome by deliberate policy. By carving out GP capacity for a relatively advantaged group, this policy stokes and promotes that law. Shame.
You may look to BMA guidance on how to dance around the policy: in essence, 25% can be for any clinician, at any time, so it could be all the HCA appointments bookable 4 weeks hence. That ensures the box is ticked, but do we really want to manage compliance by frustrating policy?
Regular readers would expect me to offer a radical and practical alternative, and I’ll try not to disappoint.
We believe that 100% of patients should be able to get help online. And we believe that 100% of patients should be able to get help by telephone. Same goes for walk-ins.
How so? It’s all the same capacity, none is reserved for any group or mode of contact. The point is that a patient can’t reserve any GP capacity, it’s up to the GP to decide what is the best way to help. Patients can request help by any mode, but all requests go into the same flow at the same time, managed by the GP according to need: none has an advantage.
We are concerned to make life easier for both patients and GPs, and we know that online requests are much faster for GPs to deal with so we encourage patients to go online. It turns out that the 25% figure is unambitious. The lowest rate of online requests for any of our total flow practices is 35%, and the average 56%. I visited one in a perfectly ordinary part of Wigan last Wednesday which gets 75% online. That’s Wigan, not Westminster.
Median time to complete a requests at the practice, Shakespeare Surgery, is 31 minutes (if they need to be seen it will be later the same day).
In summary:
– patients will do what works for them, not what they are told
– online requests can work for all ages and conditions (though usage is lower with greater age)
– online is more efficient for GPs and receptionists, freeing up time for those who still need to use the telephone.
In order to deliver the outcomes we all want, system change not arbitrary targets are needed, and suddenly it makes sense to abolish the existing assumptions and methods.
We’ve added a criterion by which we judge progress with askmyGP:
The service must benefit non-users.
Harry Longman
- Published in Comment







How do patients want help from their GP? The data.
We ask patients 140,000 times each week. The answer may surprise you.
This week has provided one of those occasions when national debate is focussed on an area where we collect relevant data, and as all doctors know, effective treatment requires sound diagnosis.
A patient sending a request through askmyGP, whether online (67%) or phoning the practice, is asked for their preferred response. We’ve asked for three years and were surprised that, pre-pandemic, only 30% asked for face to face. Perhaps more surprising is that the most recent weeks show the same data at 10% asking for face to face (chart on the left, red for face to face). On the right, actual response, shows 13% are resolved face to face. GPs are seeing more patients than ask to be seen.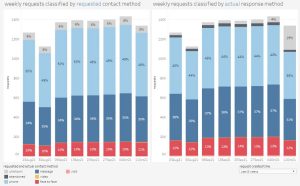
The gravitational forces on general practice underline the pressures:
– 4% growth in population over 5 years, and increasingly elderly at that.
– 5% drop in GP fte numbers, coping with increased demands post-pandemic as secondary care delays leave patients in need for longer.
Should there be more pressure to see patients face to face?
We have never expressed a view on the “right” proportion of face to face, as the clinical judgment of the GP for every patient and need is paramount. All we can do is reflect the data, and try to make the process of collecting and responding to patient requests as easy and flexible as possible, managing the whole workflow as one. GPs tell us all the time that is what they value most.
Sajid Javid said yesterday “My only target is choice” and if there’s one thing we can agree on, it’s that. Arbitrary numbers, with penalties for deviation, cannot be consistent with clinical choice or with boosting morale.
It is clear that going back to a 2019 GP service model won’t work and radical change is needed. A little extra cash won’t fix it, and more GPs will take years to train. Yet we know, from helping hundreds of practices, that right now, GPs with freedom and flexibility are providing a superb service to their patients, and keeping their trust.
Mr Javid, please trust and support GPs to do the right thing.
Harry Longman
Chief Executive