How will your PCN manage workflow, demand and capacity?
With the passing tomorrow of the deadline to sign up to the Primary Care Network DES a Rubicon will have been crossed for PCNs. The rehearsals are over, real money and commitments are at stake. But I want to know, how will they work?
A funding model is in place, a set of PCN duties and payments is agreed, no doubt controversially for some but that’s how it is. A list of professions is now 100% funded by the delightfully named Additional Roles Reimbursement Scheme.
But still I ask, how will they work?
Everything we do in the NHS needs to relate to its purpose which, however it is worded, amounts to helping patients overcome or manage their various medical needs and diseases.
The additional roles must be to help patients, who have needs. Which patients, what needs, when, with what measurable outcomes?
Forgive me if I’ve missed something, but the debates on funding, roles, governance and so on seem to be very far removed from these practical questions.
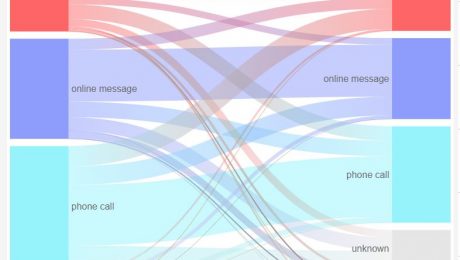
Consider the patient journey: present to GP practice, GP considers they would benefit from referral to a PCN employed clinician, say a pharmacist. How easily do they refer them? How soon can the patient be seen? How does the pharmacist manage demand from multiple practices? What is the right capacity for each kind of role?
A PCN I spoke to had a pharmacist one day per week in each of the five member practices. Neat, being five, but others will have 3, 4 or 7, and all different sizes. One may be mostly students, another elderly and with very different needs. What if our patient gets referred on Tuesday, just missing the pharmacist who calls at her practice on Mondays? And work or family commitments mean Monday never suits her?
Managing the workflow, demand and capacity for shared roles could be orders of magnitude more difficult than the same within practices.
I would love to know your thoughts on how, or ideas from your PCN. Yes, we are going to try and make it easier so you can make the most of the new resources, do let us know what you would like and watch this space.
Harry Longman
PS Last week’s blog looked at return on investment in askmyGP. David Evans replied to me that following their £35k investment in year one, they were saving £100k pa in locum costs. Not bad, indeed typical. Sujit Vasanth commented online “I can honestly say the change to askmyGP has been the most important (and positive) change in our practice in the last 10 years.” Thank you!
A number asked about spreading payments and I’m pleased to announce that we have responded with just that, it’s on the bottom of our Transform Express and it is now standard.
- Published in Comment
Why some of the best things are not free
Today I want to talk about a problem for us and for GP partners. We’ve always supported the GP partnership model as the most effective (while not the only) way to deliver high quality primary care, locally and with long term relational continuity.
Forgive me if you’re not a GP partner, no need to read on, but if you are I hope we can share some of your thinking as we are a small business with a turnover similar to a medium sized partnership. We value our independence and we want to help you use yours.
Throughout England GPs are able to access one of several suppliers free which enable them to comply with the edict to offer online and video consultations. We chose not to participate in this tender, as the allocation is random by CCG, no evidence of outcomes was required to participate and therefore it is impossible for GP partners to make an informed choice of supplier.
Not only are we competing with free, bluntly our service is around three times the price of others over 3 years. It’s a job to explain to people that it’s very different from bolt-on technology, as askmyGP enables system change like no other. We are not competing with point solutions.
This means that in addition to helping you comply with regulations, we need to sell on the concepts of “value for money” and “return on investment”. It has to be worth it for GPs making decisions as owners, those with skin in the game (I loved the wonderfully provocative book of that title by NN Taleb).
In the whole UK just four CCGs and one Welsh health board are fully funding askmyGP for all their practices, and they are flying, but let us face facts: the rest of you are going to have to pay directly. Which puts you in exactly the same position as thousands of other businesses, including ours, where investment is a decision you make to save time and money, improve your life and increase profits.
Now here is the good news: our customers are our greatest fans, and we are very grateful to them for their public support. Some recently set up a facebook group (I’ve applied to join). They are all over Twitter – last week @simondevial wrote “We’ve been using it for 8 weeks. In 28 years no other change delivered “what it says on the tin” like this.”
I was talking to Barry Sullman on Friday. He’s happier than ever after 2 years. “Using askmyGP has given my practice extra resilience, allowing us to easily cope with clinical staff shortages due to Covid, and sustain a high level of care dealing with every clinical patient the same day” He goes on to add “Last year was our best QOF year because of askmyGP. We were able to identify long term condition patients at the triage state and bring them in for care of their long term condition as well as the problem being triaged. As a result last year I reached virtually all my QOF targets before New Year’s Day!”
We hear lots like this. As a result we’re seeing the highest ever rate of enquiries from GPs, many of them unhappy with the free software imposed by their CCG with no consultation and no evidence.
However, many get stuck at the point where they need to pay, and when they are used to having everything for free, it seems odd. Yet the same people wouldn’t think twice about buying a holiday (a cost) or replacing the car (a wasting asset).
Last week my bank wrote to tell me the interest on my savings account is 0.01%. Compared with keeping £1000 under the mattress for a whole year, that’s just 10p extra, and they are threatening to charge us for looking after it soon.
I’m happy to report that increasingly partnerships are realising the very high rates of return they will make with askmyGP and deciding to invest, based on evidence, putting themselves in control of their destiny. Our practices managed 98,050 requests last week, 96% of them remotely, 69% of them received from patients online.
It’s not only the savings on locums (you will have noticed that locums are struggling to find work at present), so many echo @catiebagel’s tweet “Hope we can continue to deliver remote assessment and treatment where possible & if clinically appropriate. Often more convenient for patients and less travel has co-benefits for the environment. Agree, am so glad we had @askmygp in place before COVID hit. #greenergp”
You may have enquired with us a day, a week or a year ago. If you’re not convinced of the evidence, crawl all over our website, study our live data, ask your friends who are customers and look for independent views. If you don’t understand it yet, spend an hour on the webinar “How, but first Why, askmyGP works”.
If you’ve seen and heard enough, and you don’t want to waste a year on something free but with tiny usage and no savings, then now is the time to act for three simple reasons:
- the barriers to change have disappeared
- current workload is lower than ever
- money has never been cheaper
So many practices have got this far and then decided to hang on for taxpayer funding. They are still hanging on, six months, a year, two years later. Don’t be another disappointed hanger-on, be another delighted user, within a week. We’ve now launched close to 3% of UK practices – that’s enough to start a revolution.
Kind regards
Harry Longman
- Published in Comment
Announcing askmyGP live analytics
Britain is social distantly dancing in the street, singing to the screen and rediscovering family games behind closed doors.
Here, working away from askmyGP Towers, the nerd unit has been in hyperdrive (we’re all a bit nerdy) and we are delighted to present, drumroll,
Yes indeed, all the data from 2 million episodes, aggregated and anonymised, is in the public domain for anyone and everyone to crawl over.
- What proportion of demand arrived at all our practices last week online? 74%
- Median completion time for all patient requests last week? 87 minutes, 52% faster than three weeks previously
- Proportion of requests completed same day? 91%, up from 81% three weeks earlier
- How many patients requested a message response?
- How much has face to face dropped?
- How has patient satisfaction changed?
I’ve left some for you to explore and there’s much more.
The overall message is: access is better than ever, though very few are seeing the GP face to face. And patients are mostly very happy with that.
It’s been a full on week for us with new practice launches every day now. Delightful stories come up all the time, such as Mai, PM at Ingham, Lincs, quite moved as she explained “Tuesday was non-stop on the phones, then Wednesday we were online and suddenly, quiet like I’ve never seen in all my years here.”
A string of health boards, CCGs and PCNs have now asked us to launch all their practices double quick, across parts of South Wales, South West, Greater Manchester and Lincs. Trafford CCG is a great example, one of their practices St John’s Altrincham on our new video.
We too are being forced to unlearn and remodel how we deliver, it’s exciting!
Have a great weekend and not too much screen time.
Regards
Harry Longman
PS We decided not to be one of the 11 suppliers in the NHS England DPS online/video offer randomly allocated to CCGs. However, we were told at the NHS England webinar on Weds that there’s a “Single Tender Waiver” procurement route which CCGs can take, no idea of the details yet but let me know if you are interested.
- Published in News
For the few, not the many
After peeling 3.5kg of potatoes in just ten minutes for Burns Night, I’m grateful again to Sam Farber, creator of the OXO Good Grips peeler. Motto “Make everyday living easier.”
His wife Betsey had arthritic hands and he saw how hard it was for her to hold a peeler. The new model came after hundreds of design ideas and iterations, but despite being four times the price of its bent metal predecessor, it’s now the choice of millions of able bodied sous-chefs around the world. I would never use anything else.
What’s the connection?
My time with patients on launch day in Hyson Green, Nottingham on Thursday was fascinating. Dozens of languages are spoken among this deprived population, making it one of the most challenging places in the country to deliver high quality primary care. I submit that this is the NHS at its humane best, universal and free at the point of care for the patient in need, whether from UK, EU or anywhere else.
I watched as a Polish man created his login to make a request on behalf of his girlfriend, trying not to “help”, rather to see where there might be the slightest trip or friction. His smartphone is set to translate, but the translate bar covers one of the text windows. He needs to click “Please accept the end user licence agreement” but his fingers are fat and he misses the small checkbox. Why not have a bigger box and shorter text, “Accept the terms”?
Next I sat with a Romanian interpreter, the lady next to her not the patient but her sister, working out how to send a request by proxy, then to be able to arrange a face to face with the interpreter present.
Patient situations are endlessly complex, and we must learn how to do better for all.
It is so much harder to build something simple than something awkward to use, and it is these extreme but everyday situations that drive us continually to fine tune the patient experience.
We’d had the usual comments from the staff that askmyGP would not work for all their patients (most practices tell us why their patients are different and won’t use it). In the event 69% of requests arrived online in week one, higher than our median 63%, and the feedback has been 100% positive.
I hope the title makes sense. Design “for the few, not the many” means everyone’s life is easier.
Harry Longman
- Published in Comment
“Do you shop online?” Rural Ruskington GP moves 80% on day one
The staff room looks out over fields, a couple of hens pecking in the long grass over the fence. We’ve driven Lincolnshire’s challenging roads and arrived through quiet village streets and bungalows. Think everything Salford isn’t: elderly, stable, families and retired.
The new record set by Ruskington Medical Practice was to abolish the old and launch a completely new system from receipt of order in just ten days.
It’s the last place in the UK you’d expect to see this, but from day one they have got 80% of demand online.
They know that almost everyone under 65 has online access, and a large proportion of much older patients. The patients haven’t yet realised there’s an easier way to get help, so if they ignore the GP recorded message, the receptionist asks:
“Do you shop online?”
That simple question, almost always answered yes, means they can be directed to the website (or sent a welcome email) and off they go. Request arrives online, it’s sorted to the appropriate person, and completed within a median 91 minutes. Only 23% need a face to face or visit.
Credit to practice manager Jules for that phrase – we love simple. She’s happy, staff are happy, GPs happy, and patient feedback shows 78% say the new system is better (one aged 90), only 12 days in.
Jules tells me demand is below prediction, which I find slightly annoying as we do like to get this right.
I’ve counted and “Do you shop online?” has exactly half the syllables of “Patient Communication Strategy”. It would be funny if it wasn’t sad, but NHS England’s Patient Online programme has taken 8 years and spent countless £millions of taxpayers’ money on telling patients to book appointments online, and they’ve reached 4%.
It hasn’t worked and it will never work because GPs are smart enough to realise that allowing patients to book all their time will waste a good 2/3rds of it.
Here’s the offer that works for patients:
Tell us who you are and what is your problem, and we’ll work out how to help you. Boom.
You’d be amazed how many times GPs tell me “this wouldn’t work for our patients” – perhaps because they’ve tried something which didn’t work. That is why simplicity is so important, and why Computer Must Never Say No.
Ruskington at 80% still welcome those with no online access. Suburban Hounslow is another new launch, 86% online, Salford remain highest at 98%.
We’re looking forward to a Surrey commuter practice making the last launch of 2019 on 23rd December, and a Lincs seaside town the first of 2020 on 2nd January.
Never know who might set a new record…
Harry Longman
PS Often a fear of “opening the floodgates” leaves people torn about the risk of change. In the recorded webinar Understanding Demand we examine the evidence of what happens. Free to register.
For an idea of how the askmyGP could put you in control of your day, click here to get our four user stories.
- Published in Case studies
Digital First GP: Blackfriars Salford gets 97% online
The walk down from Manchester Piccadilly is a fascinating cityscape, and then crossing the river Irwell into Salford it seems everything is in flux.
Here, between the £180/night Lowry Hotel and the £35/night Salford Arms Hotel, lies Blackfriars Medical Practice. Perhaps that’s a metaphor for the patients Dr Babar Farooq and his team serve: young, mobile, diverse and with fortunes right across the spectrum.
It’s free to join his list and free to get help – the NHS is a great leveller.
What’s unique is that when Blackfriars launched askmyGP three weeks ago they moved 97% of their patient demand online, from day one.
There’s no messing about – Linda on reception simply tells the patients what they need to do. They send online, they get sorted within a few hours (median time to complete the episode is 193 minutes). Computer never says no.
Inside the practice with the phone not constantly ringing the drop in stress and pressure is palpable. They are bouncing. Babar keeps telling me how happy he is, and he’s resolving 38% of requests simply by message.
Patients? 86% say the new system is better. “I was surprised at how quick my question was responded to. Much faster than calling.” is a typical response, female 29.
Their demographic is young, mostly 20s and 30s, so we wouldn’t expect every practice to get this many online, 80% would be more reasonable for the average normal digital first GP.
Blackfriars in week 3? They’ve just ticked up to 99%.
Harry Longman
Pictured, between the yellow sign and the railway bridge, ground floor.
- Published in Case studies
The dark side of digital inequality
If you’re a GP you will by now be familiar with the NHS England requirement for “25% of appointments to be bookable online”. If you’re a commissioner you may be fretting about how to measure it. Anyone else is most likely bemused by another arbitrary number of little relevance.
But there’s a dark side to arbitrary requirements, and with this one it is faced by the digitally disadvantaged. We instinctively know that those least capable of booking online, for reasons of age, deprivation, mental capacity or simply being ill, are disproportionalely most in need of help from their GP.
The good Dr Julian Tudor-Hart called it the “Inverse Care Law” and it can only be overcome by deliberate policy. By carving out GP capacity for a relatively advantaged group, this policy stokes and promotes that law. Shame.
You may look to BMA guidance on how to dance around the policy: in essence, 25% can be for any clinician, at any time, so it could be all the HCA appointments bookable 4 weeks hence. That ensures the box is ticked, but do we really want to manage compliance by frustrating policy?
Regular readers would expect me to offer a radical and practical alternative, and I’ll try not to disappoint.
We believe that 100% of patients should be able to get help online. And we believe that 100% of patients should be able to get help by telephone. Same goes for walk-ins.
How so? It’s all the same capacity, none is reserved for any group or mode of contact. The point is that a patient can’t reserve any GP capacity, it’s up to the GP to decide what is the best way to help. Patients can request help by any mode, but all requests go into the same flow at the same time, managed by the GP according to need: none has an advantage.
We are concerned to make life easier for both patients and GPs, and we know that online requests are much faster for GPs to deal with so we encourage patients to go online. It turns out that the 25% figure is unambitious. The lowest rate of online requests for any of our total flow practices is 35%, and the average 56%. I visited one in a perfectly ordinary part of Wigan last Wednesday which gets 75% online. That’s Wigan, not Westminster.
Median time to complete a requests at the practice, Shakespeare Surgery, is 31 minutes (if they need to be seen it will be later the same day).
In summary:
– patients will do what works for them, not what they are told
– online requests can work for all ages and conditions (though usage is lower with greater age)
– online is more efficient for GPs and receptionists, freeing up time for those who still need to use the telephone.
In order to deliver the outcomes we all want, system change not arbitrary targets are needed, and suddenly it makes sense to abolish the existing assumptions and methods.
We’ve added a criterion by which we judge progress with askmyGP:
The service must benefit non-users.
Harry Longman
- Published in Comment
Making it easier for patients (shock!)
“The patient journey…” We are fond of that phrase in the NHS, aren’t we?
That’s in the parallel universe of politics and pipedreams. The reality when we become patients is often very different. As one GP tweeted last week “Have to say being stuck in a trolley queue for over 3 hours got me thinking about patient flow”
At a practice on Wednesday a receptionist told me of the time she had a patient across the counter and had just explained they had no appointments left. He pulled out a pink screwdriver and started waving it at her. In that situation you would remember the colour of the screwdriver, though I was unable to see why a screwdriver would change the availability of appointments.
Wherever you enter the system, it can be deeply frustrating, when you know what you want and just can’t seem to get it. The patient journey we all want is one that works, and if it did, the NHS would be far cheaper to run.
We have a shockingly radical thought: “Make it easier for patients to get help”.
In general, most of us now start looking for local services online. That means the GP practice website is the very start, and what could be more important than getting this right?
Having looked at hundreds, they fall into three main groups:
1. Standard commercial offerings – low cost templates, everything included, ticks all the boxes.
2. Boutique designs – beautiful graphics, videos and moving images, where what you want must be somewhere…
3. Push-you popups – wherever you go on the site, they tell you what you want and it’s very hard to find a way around.
The problem we felt with all of them is that they don’t help the patient find and do what they want to do.
We don’t do websites, but we found someone in Tim Green at GPSurgery.net who does, and starts with patients. He tells me that most patients click on:
– how do I get an appointment?
– repeat prescriptions
– meet the team.
Aha. So that’s exactly what we put on the home page of our patient demo site Bramley Surgery.
Do try it, and we would love your feedback on the patient journey. Send in a request and we might even reply (sorry, no actual medical help).
Here’s the news: we have bundled one of Tim’s wonderful websites free with our Transform and Improve Pro packages. You can stay with your old site, but making it easier for your patients turns out to have a beneficial side-effect.
With 57% of demand now online, they make life much easier for you too.
Regards,
Harry Longman
- Published in Comment
Ben Gowland talks to Hugh Reeve
Delighted to share a surprise with you which I first heard on Wednesday.
Many of you will know Ben Gowland of Ockham Healthcare and his regular podcast.
This week he interviewed Dr Hugh Reeve of Nutwood Medical Practice in Grange-over-Sands, Cumbria. It’s 25 minutes of straight-talking on why they implemented askmyGP and what happened.
I’ve learned a lot from it too, about the importance of continuity for GPs as well as patients. As Hugh says, it pained him when patients had to wait days to speak to him, or were then passed around to others. Rework was bound to follow.
I love the bit where he says it’s not a bolt on, and where he says after 6 months each GP has shaped it for themselves. This is one of the most elderly populations in the UK, and they are now at 40% online. Quite a story.
Harry Longman
PS Do sign up to get Ben’s regular blogs.
Patient feedback:
- Published in Comment










Putting two and two together on GP workload
Like many of you I’ve joined in the clap for key workers on Thursday evenings, and very well deserved it is too. There’s little doubt in the public mind that the NHS has performed better in the pandemic than the government overall.
But working in the health sector we have every reason to feel not just pride but relief, as we are in relatively secure jobs while we see others all around lose their livelihoods in everything from hairdressing to aerospace.
This week another survey comes out from the BMA, GPs bemoaning their lot for one reason or another. In the eleven years I’ve been working with GPs, something like this appears almost weekly, predicting the end of the profession as we know it. Yet the GPs we work with are more secure than ever, loving the job and have never been better off.
Adding to the conundrum is disturbing data on numbers. As reported in GP Online, GP ftes are down 712 in the year to March 2020, and GP partners down 1,023. Yet in the same issue, GP locums bemoan the sudden loss of work in the pandemic, 81% seeing a drop in income.
I’m sure that, like me, you have many friends and relations in the medical profession and I’m sure that considered overall you wouldn’t disagree with what one observed to me, “We’ve never worked less hard since we left medical school.”
It’s amplified by leaders saying “We’re not going back to the working life we faced before the pandemic”.
I can’t wait to be rid of the restrictions on all our lives, but there’s little doubt that general practice will not return to the working format pre-covid. RCGP reported that face to face had dropped to 25% of consults, which seems high to me as our practices dropped from 30% to 2%. It has now crept back to 5%, while total demand is nudging up towards pre-covid levels.
Having discovered the efficiency of telephone triage overnight, partners will not offer face to face to everyone again, rehire all the locums and take the hit on their profits. We’ve been saying this for ten years, a few pioneers have said so for twenty years. Our latest askmyGP data, live here, shows 37% of requests are now resolved by message alone, no need even to telephone and much more time saved, while patient feedback is up too.
Practice after practice is discovering the same, but they all seem to go through a ritual of catastrophisation before they launch. At one this week the GPs were very adamant that Friday would be the busiest day, and I said they would remain very adamant until Friday. It came in with less than half even my predicted volume.
Another due to launch next week did the staff survey, and the biggest fear of the partners was higher workload. The biggest fear of all the other staff was losing their jobs because of lower workload. It’s a GP thing, and it goes with the territory.
With the huge extra resources now going into Primary Care Networks, I foresee very good times ahead for GP partners. If you’re a locum or salaried, apply as soon as you see a good opportunity. If that translates into better patient service, better quality and continuity of care, and more fulfilled professional lives, we all win.
So I’m very optimistic, but honestly, I’m bored with lockdown. I haven’t quite reached the point of sorting out my sock drawer, but I’m close, and that’s serious. Okay okay, “There’s never been a better time to sort out my sock drawer.”
Harry Longman