Game on, Babylon
Have to say it makes one a little queasy to see the Secretary of State take the platform at a competitor HQ and tell they world he wants their product to be offered to everyone. Taking a few shortcuts on procurement, open competition, evidence and so on, but then he’s new.
Two things I share with Matt Hancock are his enthusiasm for how technology can help, and his frustration with the glacial rate of innovation adoption in the NHS (plenty of innovation does not equal high rate of adoption).
But we absolutely must see technology within the whole system context, which is why we call what we do “Systems thinking applied to general practice.”
Mr Hancock might like to consider a few matters before handing over the jewel in the NHS crown to Babylon’s GP at Hand:
– their patient profile is skewed to younger adults
– they’ve traded access for discontinuity of care
– their exclusions, agreed by NHS England, cover children, pregnancy, many chronic conditions, those who can’t travel, pretty much most of the demand on GPs.
– taking out the above patients leaves remaining GPs with most of the work but much less of the income.
He’s right that a quick query on an acute illness from the back of the ministerial Jag could and should be dealt with online (if appropriate) by the patient’s own NHS GP. But from the GP side, that’s a very small segment of demand.
I fear a sinister side to the Babylon gig on Thursday: BMJ reports that Ali Parsa is lobbying NHS England not to cut funding for “digital first” GP providers out of area. Well he would say that, but having the SoS publicly tout your product is quite a nice negotiating gambit.
We aren’t just going to rail at the darkness. It would be lovely to have the endorsement of the SoS but until then, we’ll let the evidence talk.
- Practices running askmyGP serve about 8 times as many NHS patients as GP at Hand.
- Last week they did 6,600 online requests, probably 3 times as many as GP at Hand (and twice as many as eConsult, who claim 500 practices now to our couple of dozen)
- All patients had a choice of their own GP.
- They are digital first but never digitally exclusive – patients are able to use the channel that works for them.
- They get a faster service than Babylon can do, response in minutes and face to face same day.
- No patients are excluded from the GP list or turned away.
Call it disruptive innovation if you wish, but we’re disrupting the operating model, not the business or contracting model. That’s why GPs love it.
Parsa announced on Thursday another $100million investment into his company to be spent on AI, on top of the $60m already sunk. I don’t know whether this has been systematically reviewed, but it couldn’t recognise my fungal toenail infection. More seriously, @DrMurphy11 has shown how it misses a “barn door PE”.
I’m announcing today a secret weapon in askmyGP. We call it HI. It’s used for every single clinical diagnosis and decision, and even better, it does care. It can care for any patient, even one deaf, blind, lame, foreign, depressed and pregnant all at once. It understands context, nuance, subtlety, ambiguity, the importance of relationships. It even takes responsibility.
We work with over 100 GPs and I can tell you, each one is worth well over $1million. So much we can’t measure it.
Something else you need to know about GP at Hand, which is why they worry so much about funding per patient. Their Achilles heel is operating costs, sky high, compared with regular partnerships offering digital first. Drop me an email to find out how we know.
Our mission is to enable regular local GPs to outcompete Babylon, online, on quality, service and profitability. We’re showing how any practice can do it. We’re growing multiple times faster than GP at Hand, adding another 20,000 patients this week.
Someone will notice before long. A GP copied me yesterday her invite to Mr Hancock to come and see askmyGP in action.
Game on, Babylon.
Harry Longman
PS A North East practice launched two weeks ago and has already blown my socks off as well as its own. They’ve gone from a median 5 day wait to see a GP to median completed request in 70 minutes, and demand went down in week 2.
One of their 91 year old patients commented, “Excellent, this service should have come earlier”
- Published in Comment
Do not use in emergency
Do you glaze over when they report the latest A&E statistics? It’s all about what % of patients were seen within four hours. The latest figure for July is 89.3% and while it produces a lot of headlines, gnashing of teeth and calls for more resources, the saddest little note in the NHS England Statistical Commentary is where it says, “The 95% standard was last met in July 2015.”
Readers of this column know that I’ve been campaigning against the target culture that grips the NHS for many years. For me the personal journey was working in manufacturing in 1990 when I came across the work of W Edwards Deming, who said we must abolish all numerical targets. I fought against that thought internally as I tried to come up with ever cleverer targets for the factory, to cover all bases of timeliness, efficiency and quality. Until I crumbled – they could never work.
Nearly thirty years later we have this regime in the NHS which daily makes hard working professional people feel like failures. It has seen off a string of hospital chief executives who were either unlucky enough or failed to cook the books enough to keep their impossible jobs when the inspector called.
Measurement and accountability matter, but they are completely different from targets. Just briefly, let us suppose that the time to be treated in A&E matters – well I think it does – we can measure the median time, and chart it day by day, week by week, ever so simply. Everyone can be engaged in improving the system which will show in this and other appropriate measures. Fear of failure is replaced by pride in work.
I’m building up to some quite astonishing news but while we are on the theme, similar thinking is applied to ambulance response times. Red C1 and C2 calls have to get a response in 8 minutes 75% of the time, and there’s a vast bureaucracy, dreaming up and calculating the numbers and beating up the failures. Sigh.
Back in the GP world thankfully there are not so many high profile arbitrary targets (arbitrary ratings on arbitrary measures by CQC are another matter) but there is related anxiety about some of what we do. We get asked “How does your online askmyGP system handle red flags?” I assume on the basis that the patient may have something urgent wrong with them.
My answer is always the same: “Red flags are dangerous because algorithms cannot completely and safely cover all eventualities, yet they can give a false sense of security.”
Because we are very concerned about patient safety, we have a different approach, which is to understand that safety is a function of the system as a whole. Rapid response by a GP, appropriate to the patient and their condition, is a very safe system. Oh, and we make it very clear to the patients, “Do not use in emergency.”
We are also very clear on what they can expect, which is a next day response out of hours, or in working hours “usually within the hour.”
When GPs doing our Pathfinder diagnostic hear about this they often blanch and explain how they would water this down as it’s clearly impossible. And then we look at the data.
So here is the astonishing news from the first two practice launches with our new software (no, you didn’t miss anything, we haven’t announced it yet). In the first week of operation they achieved a first response average time respectively of 6.0 and 5.2 minutes.
That’s a personal response from a GP who has seen their request and triaged how to help (a face to face may come later). But it’s average, all demand, not just what someone considers urgent. No blue lights, no inspectors, no targets, no pressure, no overwork, no rework, just ordinary GPs, predictable demand and good flow.
Have an ordinary weekend.
Regards,
Harry Longman
PS Dr Simon Wade of Webinars for GPs has invited me to present this Wednesday 22nd August 8 – 9pm. Do join us on “Workload stress and burnout: can online access make a difference?” CPD points too!
- Published in Comment
GP pay, rations and recruitment
No doubt your inboxes have been weighed down with the debate on the “2% pay rise for GPs”. Is it 2%, 1%, 3.4% or 4.2%? Of course it’s nothing of the sort.
It’s a contract uplift to independent contractors. If you buy a pencil, it comes out of your drawings. If you save a pencil, it goes into your drawings. I’m afraid the general public don’t understand this, but never mind.
There is no perfect model and of course it has its drawbacks, but I think the ability to run your own business is one of the great strengths of UK general practice. GPs have huge freedom to determine their own business performance, and therefore their profits and drawings.
Alongside improving patient service, one of our explicit goals is to make GP practice owners more profitable. Some of you seem rather coy about this, strangely, but I see it in very simple terms: why else would you pay us?
Because business owners take home the difference between income and expenses, they know that they can increase their incomes vastly more than 2% by investing in a machine to make pencils – I’ve over-extended the analogy.
Pencils are cheap but the expensive bit of the GP business is the GP. So the game is to make the GPs 30% or 40% more productive.
We are drawing near to Hancock’s Holy Trinity of “improving outcomes, helping clinicians and saving money”
Meanwhile there’s a monstrous failure: NHS England can’t persuade enough foreign trained GPs to come here. They wanted 2,000 no doubt at vast expense, and they are under half the target. They are looking in the wrong place. We already have the GPs. And by enabling them to be more efficient, and more profitable, we’ll have plenty.
It is a national scandal that a developed nation should steal the trained workforce from other countries who may have far fewer GPs per head than the UK.
We can do better.
Regards,
Harry Longman
PS I loved this tweet earlier today from @dave_dlt “Heck of a day, 4 sessions down then one partner needing to get away unexpectedly yet 1650 building calm and quiet”.
We are seeing partners shed locums and salaried sessions then still get away on time and enjoy the sunshine dividend.
- Published in Comment
Matt, meet Aneurin
Who’d have thought it before the Chequers meeting, but there it is, we have a new health secretary. I’ve put together some words from the very latest, and the first, of those at whose desk the NHS buck stops.
At the start of Matt Hancock’s term those interested hang on to every word, but to save time I’ve cut and pasted what I find most relevant here:
“as you may have heard I use an app for my GP. The discussion around my use of a Babylon NHS GP, which works brilliantly for me, has been instructive.
Some people have complained that the rules don’t work for care provided in this revolutionary new way. Others have said the algorithms sometimes throw up errors.
Emphatically the way forward is not to curb the technology – it’s to keep improving it and – only if we need to – change the rules so we can harness new technology in a way that works for everyone: patient and practitioner.
I want to see more technology like this available to all, not just a select few in a few areas of the country.”
A lot of positives. Sees the potential of technology (the NHS is so far behind, he could hardly not), brings in personal experience. Wants universal coverage, hear hear.
Steps into controversial territory with a commercial namecheck perhaps, but there’s a precedent. What I suspect he doesn’t understand is that GP at Hand while limited to the London area at present is not and cannot be a universal model. They exclude a long list of those most in need of a GP, as I don’t need to remind you, and they can’t offer continuity of care.
Our approach is rather to enable existing GP providers with local access and coverage for all patients, to give a much better service, much more profitably. We already serve about 8 times the number of patients covered by GP at Hand, but you might not think so by the volume of noise.
In recent week’s we’ve seen a growing body of GPs tweeting to let the world know that it’s really working. If you haven’t seen it do join the conversation, click to follow @askmyGP
Now to Aneurin Bevan, who wrote to the profession on 3rd July 1948:
“There is nothing of the social group or class in this: and I know you will be with me in seeing that there does not unintentionally grow up any kind of differentiation between those who use the new arrangements and those who, for any reason of their own, do not….”
We can say without fear of contradiction that all parties are agreed on that. The question is how, and what policies could threaten it. Bevan continues
“My job is to give you all the facilities, resources, apparatus, and help I can, and then to leave you alone as professional men and women to use your skill and judgment without hindrance.”
I’ve no doubt that 70 years later Bevan would be banging the table to say we had better get up to date with the means of doing so.
“Skill and judgment” – that’s human intelligence and in relating to, diagnosing and caring for patients, AI algorithm chatbots can’t hold a candle. Someone telll [email protected].
Harry Longman
PS Babylon’s recruitment page says its GPs “will see up to 5 patients an hour”. Jaw hits table. Our GPs tell us they would collapse with such a poor rate of producton. Looks even more like the Babylon business model can’t cope with anything but a fit and healthy demographic.
- Published in Comment
Improve continuity, die less often
Did you hear the wonderful piece on Inside Health yesterday as Mark Porter interviewed Sir Denis Pereira-Gray? Listen on iPlayer from 4:40 minutes.
Sir Denis has been a tireless campaigner for relational continuity and his new paper published in BMJ Open. is the first systematic study linking better continuity with reduced mortality. Boom – the doctor knows the patient, they are likely to live longer.
But as he points out, continuity is actually falling, by an astonishing 27.5% between 2012 and 2017 as measured in this Leicester paper.
This is not inevitable.
It is the consequence of policies, system design and operational practice.
Therefore reversing the decline is a choice. The question is how?
Working with a huge range of GP practice structures and sizes, we have a very simple method.
- GPs set up their availability
- Patient chooses named GP
- Reception assigns patient to GP.
The data is interesting – only 25% of patients name a GP and quite often reception will look up the usual GP and assign to them. But most patients don’t mind and where it doesn’t matter, this gives enough flexibility to share the workload evenly.
It all happens within the normal flow of the demand led day, and crucially patients who feel their need is urgent are not faced with the dilemma of “You can see the duty doc today or that one you want in 3 weeks”
Now all of a sudden there’s a way to convert this into money. There always was, since continuity improves efficiency as GPs sort things out once properly, and patients don’t create rework.
The new time limited way is thanks to the Health Foundation launching a programme to increase continuity in general practice.
All excellent stuff and I wish you well.
Harry Longman
- Published in Comment
Don’t fall into the specification trap
Another week, another specification thumps onto the floor in front of my inbox. NHS Blithering CCG* has copied down the questions from the last lot, added the requirement to integrate with local place-based cloud-enabled remote home visits by Longstay (Vietnam) NHS Telecare plc, and there, ta-da, is the blueprint for online consultations.
As I read through the same tired wishlist, my heart sinks. Must have:
- red flags (unsafe and cut patient use by around 60%)
- symptom checkers to divert patients away (unsafe and patients hate them)
- ability to book GP appointment (wastes GP time as 70% of patients don’t need a face to face)
It goes on, and of course we aren’t going to rewrite our software to meet this specification and thereby ensure it doesn’t work. What’s missing from the list are many of the features which really do matter to patients and GPs, let alone any serious understanding of the journey of change which is much more expensive to deliver than software.
If the CCG has decided on a tick box procurement process, we’ve put ourselves at a serious disadvantage. We run a permanent policy of not lying about evidence, rather presenting the raw data and letting the customers talk about the outcomes. Worse still, we don’t promise the moon unless we have clear technical and economic means of reaching the moon. Overall disastrous.
So I’m going to ask you a genuine question, if you’re in an English CCG, or a GP affected by the DPS procurement process through the ringfenced £45m online consultations fund, set up by Arvind Madan, former eCONsult chief executive: should we pull out of the DPS?
CCGs can still procure askmyGP or any competing product via G-Cloud, and draw on the same £45m fund. We are fully compliant on patient safety, information governance, security and so on. But our product development is driven by the simple question “what works?” rather than “what is specified?”.
It’s a philosophy that has enabled orders of magnitude greater usage and value for patients and GPs.
What those tick boxes and essay writing competitions can never ask is whether it will do this. Copied to me yesterday by Dr Barry Sullman, writing to another GP and he’s delighted to share:
“AskmyGP is a revolutionary system, that has transformed my work/life balance. It is now normal for me to have breakfast, and tea with my family. It has also transformed care at the surgery, empowering patients, and creating efficient SAME DAY care.
But I don’t want to talk hyperbole. I want you to come and see this on a live system, where you can see this really happening. I have recovered the cost of the system in 3 months, and I will continue to recover the cost many times over indefinitely until I retire. Let me show you the math when you visit.
This is the future – and doctors need this sorely as do patients.”
So what do we do? Advice welcome or if you like put it in public and comment online.
Harry Longman
PS Wales and Scotland do not suffer the same procurement blight as England and they are pulling ahead, as are English GPs investing in their own businesses for the return Barry mentions above.
*Blithering and its staff are an unregistered trademark of the great @jtweeterson, used without permission. The genuine article is here.
- Published in Comment
The vision of Julian Tudor-Hart
At the end of a week of “fun” on the NHS at 70, I want to contrast two views of what it’s about.
Matthew Parris is always thought provoking and he writes today in the Times, “The NHS guarantees second rate healthcare”
In case you don’t have access through the paywall I’ll summarise his thesis. Transport in London is slowed by congestion to the point where people would rather walk. When it speeds up, they will get back in the car/bus/tube. NHS Healthcare is like transport, keeping the waits long and the service cumbersome is a crude way of rationing. If we made it faster, more patients would jump in to the point where it slowed again.
“We’re getting a second-rate health service for the price of a third-rate one. I see no other way.” Meh, as my daughter would say.
The theory is impeccable, just spoiled by an inconvenient fact: it’s not true of healthcare. Easier access doesn’t increase my number of diseases. If the theory were true, lowering the effort to access the GP as close as we can to zero would see demand escalate.
It doesn’t happen. Demand is flat. Patients don’t even need to wait for the phone to be answered, and they are getting a personal response within minutes.
Witley yesterday: “our waiting time for routines is now half an hour. And we’re a partner down this week, unplanned.”
You may have heard of the death last week of Julian Tudor-Hart. So much has been written about him and by him on the NHS, I’m grateful to @mellojonny for a 9 tweet summary (click Show this thread). He starts with “1. A united national service devoted directly and indirectly to care, fully available to all citizens.”
We never met but at 85 he wrote to me in 2012 and I quote:
“So I count on you & others like you to carry whatever is useful from my torch, which I in turn got from my predecessors – my father, Len Crome, Hugh Faulkner, Alistair Wilson, Jerry Morris and a small handful of others.
I wish I could get more people to read the 2nd of my Political Economy of Health Care, especially the final chapter. To act effectively and sustainably throughout their lifetimes, people must have a comprehensive big picture of society, and how fundamental social change actually works. So far, very few people have that. Until they do, we and our descendants will be in mortal danger, worse than 1933-45.”
Matthew Parris or Julian Tudor-Hart: choose your vision.
Regards
Harry Longman
- Published in Comment
The blood test, my story
I’m fortunate rarely to need the NHS, so when I do as this week there is so much to learn. And it touches directly on why we can routinely make life changing efficiency gains in the order of 40%.
Where could that possibly come from in practices who tell us the whole time they are bursting, sinking, drowning or whatever hyperbole they choose? They can only see one way out, recruiting more GPs, and they can’t recruit.
So here’s my story. I need a blood test for schistosomiasis after swimming in Egypt, as another member of the group tested positive. While I explain what happened, tot up in your head the waste…
Weds 27/6 I check online to book an appointment, next available is Friday 29/6, HCAs only this week, but I think, blood test, will be OK, and clearly state the reason.
Friday 29/6 Three phone calls around 8am, all of which I miss, but get a message and call back. HCA can’t do this one, could I see nurse instead, and she’s free at 11.30. I grumble, shorten a meeting and agree to go at 11.30. (wasn’t available to book online)
I’m on time, but she spends the next 15 minutes explaining how unusual this blood test is (me: “but I’ve only got one kind of blood”), nips out to refer to GP. Can’t take the blood, but GP will call me today at 4.30 to explain what needs to happen. (slot wasn’t available online)
4.30pm GP calls and spends 4 minutes explaining what the nurse told me, and that I now need to book another appt with an HCA to take the blood. (what really creased me up was seeing the note online for my 10 minute call: “This was a difficult pt earlier”. Not intended for my eyes!)
Monday 2/7 I book another appt with HCA for Friday 6/7. Today I turn up at 11.50 and the HCA takes my blood, I’m out in 4 minutes and the actual value work is done, at long last. I was a very brave boy and got a badge.
I did everything by the book, all online as Jeremy Hunt wishes, but did you tot up all the waste? 4 receptionist phone calls, only one connected. 15 minute nurse appt, including an interruption to the GP. 10 minute GP slot, achieving nothing.
You missed something – over an hour of my time.
I can hear you whispering that this was a special case but do you know, for the patient every episode is a special case? Other family members get a similar run around pretty much every time they need help from the GP. Then they try going around the system, just because they are human beings, just like all the other human beings who tell me daily about their frustrations.
But have you seen how the magic works?
All we need to do is take out the waste and rework.
I’d go online with askmyGP, answer a few questions to explain exactly what I needed and send. Looks complicated, receptionist assigns to GP who in total peace and quiet looks up the procedure in seconds and messages me to say come in for the blood test, today. Done.
Multiply hundreds of times per week for each practice and millions of times per week for the UK.
Jeremy Hunt wants to automate the waste, creating more waste. Andy Burnham pops up to tweet “This lazy line that the NHS is inefficient annoys me.” That’s not lazy, it’s caring. I counter with Don Berwick: “Efficiency is a moral imperative”
Most of us will be born, live and die cared for by the NHS. That doesn’t make it a religion, just a jolly useful health service. Britain has sadly become one of Europe’s most unequal nations, and the NHS does a little to level opportunities at least in one sphere of our lives.
The NHS at 70 doesn’t need reverence. It needs principled leadership, critical friends, and no-nonsense doers with method.
Harry Longman
PS If you’re sick of all the hearting, @jtweeterson’s blog is guaranteed to cure you. Simply brilliant. Sit down first.
PPS My story above shows why our first question in Pathfinder is “What is it like to be a patient? The data we capture make that pretty clear, and it helps to focus on purpose, good preparation for the next step of eliminating the rework.
- Published in Comment
Appy Birthday NHS 70!
I’ve no doubt Jeremy Hunt meant well by what he called his birthday present to the NHS, a new NHS app. But as W Edwards Deming said, “Best efforts are not enough, you have to know what to do.”
“I want this innovation to mark the death-knell of the 8am scramble for GP appointments that infuriates so many patients.” says Hunt.
He’s right that innovation is needed, right that there’s an 8am scramble and right that patients are infuriated. One phoned me this morning, absolutely fizzing about her practice, but not one of ours and there was nothing I could do. She told me she could book online, but there were never any GP appointments soon enough so she physically went this morning and still no joy.
The gap is in understanding the problem: it’s the system. It’s not lack of online access, standard for some years. Bad news, it’s the system, meaning the operating system of the practice. Good news, it’s the system, meaning it can be changed. By whom? The GPs who run the practice.
Even better news, it isn’t a matter of resources. The BMA is right that Hunt’s NHS app won’t create any more appointments, but their knee-jerk reach for the begging bowl so lacks imagination.
I won’t bore you with how we are helping practices to achieve 30 – 40% efficiency gains, and help patients within minutes, because you’ll tell me it’s too good to be true.
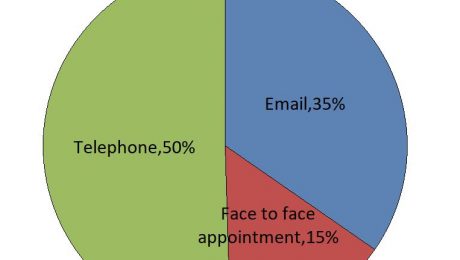
But I’ll share with you a brand new chart which astonished me this week, and it goes to the heart of Hunt’s problem definition. A month ago we started asking every patient when they send in from askmyGP how they would like the GP to respond, whether email, phone or face to face. This is from 12 practices who have done Transform, online varies from 15% to 80% of demand, average 35%.
Even though around 30% of patients need a face to face, only 15% are asking for one. GPs are having to persuade some patients to come in.
It seems obvious after all: patients don’t want an appointment, they want help with their medical problem from someone they trust.
But if you make it a thing to book appointments online, then that’s what they will do, and take 10 minutes of GP time, even though neither party wanted it.
The BBC listened, thank you, and we have been saying this to NHS England for a long time, but they aren’t listening. Can you help?
Harry Longman
PS #GarethSouthgateWould not mention that 6 out of 9 England goals have been scored by a Harry, so neither would I.
PPS All the above practices started with Pathfinder – Could you be ready to change? It’s normally quiet in summer but we are surprisingly busy and it is actually the best, quietest time so do get in touch today.
- Published in Comment







A climate of change
I’m sitting here in my shorts, tee shirt and sandals and it’s the middle of October. Yes, I’m in Leicestershire, for those thinking laterally, and I have a jumper on, but I felt it worth dressing up to make the point.
Unless you’ve already settled on Mars, you’ve noticed that it’s significantly warmer than in your youth and while a fine warm week in October is weather rather than climate, we know the trend is one way.
The IPCC warned this week that our fossil fuel burn must fall more rapidly than we thought. Policy must change, and behaviour must change.
We link our work with askmyGP directly to lower carbon use, because it saves travel to the GP surgery. It’s hard to measure the numbers with telephone consulting, but we have much better data now with some 10,000 patient requests via askmyGP each week. Roughly 9,000 are for the GP, of which 6,000 are resolved remotely. Say half would have involved a car journey of say 1 mile each way, that’s 6,000 road miles saved – and we have only just started.
I’m optimistic that if we do the right thing, a lower carbon future can be a better one all round, and I’m glad to say the patients agree.
“Fantastic service, much easier to speak to GP whilst sitting in the comfort of your own home. Many thanks” f 53
“So much better than getting in the car and visiting. Personal chat with my GP at a time convenient to us both.” f 65
“I think the new system is excellent. Saves time and must give the doctor more time to see patients who actually need proper medical attention. Saves me from having to bundle my 1 year old son on a bus and come up for nothing. Love the new system!”
And why should patients have all the fun? One of our practices has instituted a work-from-home-day for all the partners. They are as productive as ever if not more so, one telling me she saves a 50 minute car commute each way.
GPs keep telling me they are terribly stressed, and I’m sorry we don’t do counselling or mindfulness sessions. All we can offer is to change the system, but consulting in slippers is quite nice.
Anyway, if you haven’t yet seen it, listen mindfully for 25 minutes as
Three GPs Spill The Beans
Warm wishes,
Harry Longman
PS. When each request is completed, we invite the patient to leave feedback and about 5% do so. The real time chart shows about 3 to 1 say the new system is better v worse, but one wrote this yesterday which was moving:
“It’s more than better. This is revolutionary. No waiting to see a GP and the speed at which the service delivered is outstanding.
I’ve switched practices to Central….the doctors are way above my previous experiences with another practice” m 67.
Another patient yesterday wrote the longest comment we’ve ever seen, an essay. I’m going to publish it tomorrow, do look out.
*Featured image is one I took in a GP car park, the environmental consequence of “GP at scale”.