Who chooses how a patient sees their GP?
It’s a hotly contested topic. Data on what happens might help.
England’s Health Minister Sajid Javid said this week “Where patients have a desire to be seen face-to-face, and this has been an issue recently, I think that choice should be respected.”
Many would agree from both the patient and GP perspective, and respect should be at the heart of the relationship. The rub is when respecting choice becomes compulsory, and here the GP profession is loudly objecting. The GMS contract is silent on the mode by which patients are helped, the professional discretion of the practitioner being paramount.
So how might data inform the debate?
In the previous blog we looked at choices made by patients on the mode of response they would prefer, from the weekly 140,000 askmyGP requests. We can then track what happens to each one, as the GP or other practice staff member records the actual mode by which the request is completed.
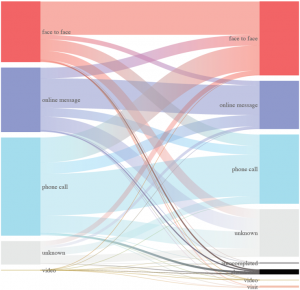
The Sankey chart is an analytical joy, named after Captain Sankey in 1898 for his steam engines, earlier made famous for illustrating Napoleon’s 1812 Russian campaign. Adaptable to the flow between stages of any process, it brings instant illumination. It’s exactly what we need here to show the flow between patient preference and outcome with the GP or other staff.
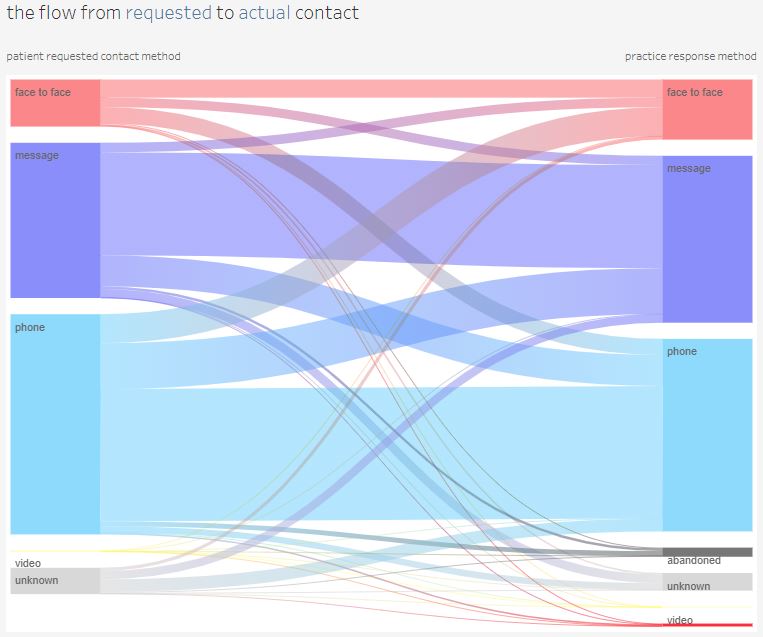
The key points on face to face consultations:
– more patients had a f2f than asked for one
– only one third who asked for f2f got one
– most of those seen f2f had asked for telephone, and many only for a message response
What if patient preference ruled every time?
The data suggests the proportion of face to face would go down, and a number of patients would not be seen, because they asked for a telephone or message response. Of course, we can’t be sure what would have happened in an imagined scenario.
What is clear from the data that is that GPs are making the clinical choice to ask patients to come in even if they don’t want to.
As a patient, isn’t that exactly what you would want?
As a GP, isn’t that the discretion your work requires?
Harry Longman
Source: askmyGP live analytics
- Published in Evidence
How do patients want help from their GP? The data.
We ask patients 140,000 times each week. The answer may surprise you.
This week has provided one of those occasions when national debate is focussed on an area where we collect relevant data, and as all doctors know, effective treatment requires sound diagnosis.
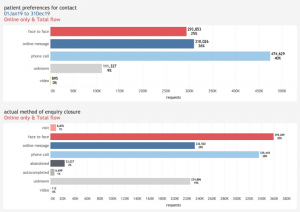
A patient sending a request through askmyGP, whether online (67%) or phoning the practice, is asked for their preferred response. We’ve asked for three years and were surprised that, pre-pandemic, only 30% asked for face to face. Perhaps more surprising is that the most recent weeks show the same data at 10% asking for face to face (chart on the left, red for face to face). On the right, actual response, shows 13% are resolved face to face. GPs are seeing more patients than ask to be seen.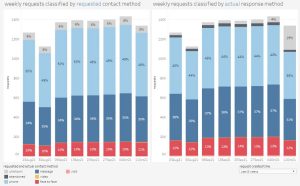
The gravitational forces on general practice underline the pressures:
– 4% growth in population over 5 years, and increasingly elderly at that.
– 5% drop in GP fte numbers, coping with increased demands post-pandemic as secondary care delays leave patients in need for longer.
Should there be more pressure to see patients face to face?
We have never expressed a view on the “right” proportion of face to face, as the clinical judgment of the GP for every patient and need is paramount. All we can do is reflect the data, and try to make the process of collecting and responding to patient requests as easy and flexible as possible, managing the whole workflow as one. GPs tell us all the time that is what they value most.
Sajid Javid said yesterday “My only target is choice” and if there’s one thing we can agree on, it’s that. Arbitrary numbers, with penalties for deviation, cannot be consistent with clinical choice or with boosting morale.
It is clear that going back to a 2019 GP service model won’t work and radical change is needed. A little extra cash won’t fix it, and more GPs will take years to train. Yet we know, from helping hundreds of practices, that right now, GPs with freedom and flexibility are providing a superb service to their patients, and keeping their trust.
Mr Javid, please trust and support GPs to do the right thing.
Harry Longman
Chief Executive
How do access hours affect online GP demand?
Demand in general practice is high for the time of year, not just in the media but in the data. It may result from a combination of changes coming out of lockdown, delays in secondary care or easier access, but we don’t have convincing evidence of which is most significant.
The question of what to do about it can’t be separated from the cause, as a wrong diagnosis and resulting wrong solution may make the situation worse. Some have speculated that easier access online is driving up demand, which sounds logical although we saw no evidence of that pre-covid. Nevertheless, if better access has uncovered unmet need that was there all along, what should be done?
One suggestion is to reduce the hours in which online access is available, and Steve Black has taken a look at the outcomes in terms of total demand as a % of list size, since the start of 2021. In the first example, online is available 24/7, although patients are told if they are out of hours to expect a reply on the next working day. Grey bars represent availability, and the red line shows total demand.
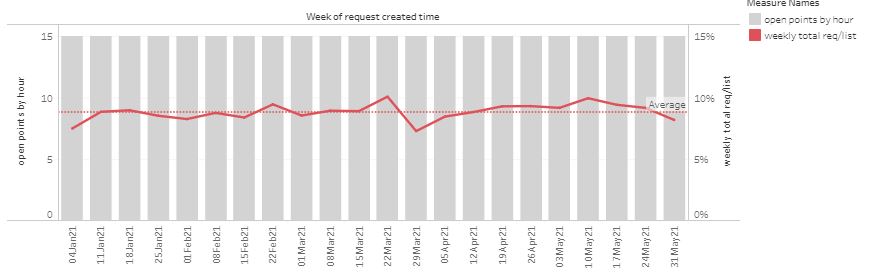
“Open point” is a score based on the period when patient requests can be submitted, weighted towards normal contracted hours. The red line is total demand (online and telephone requests) as a % of list size, per week.
In the following example, opening hours were cut in response to perceived high demand.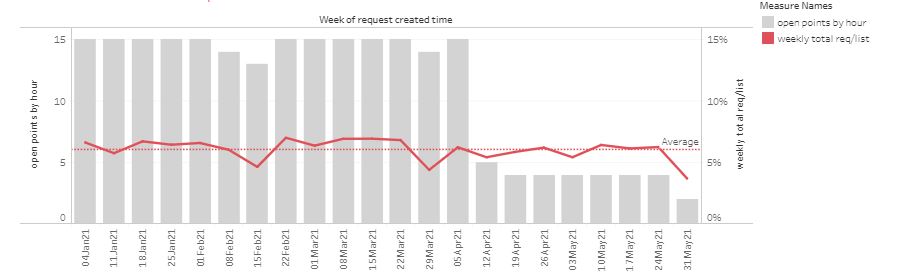
Another practice has made multiple changes in an attempt control demand, sometimes significantly reducing availability even in-hours.
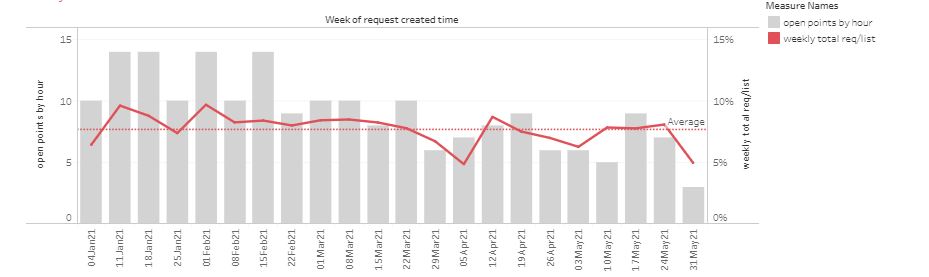 Overall, changing opening hours has had little effect on demand. However, as a patient there is a loss of service as they cannot be so sure they can submit a request online when they want to. Constantly changing the time the system is turned off risks patients losing trust in the online route, driving more demand through the telephone route which is less efficient to manage.
Overall, changing opening hours has had little effect on demand. However, as a patient there is a loss of service as they cannot be so sure they can submit a request online when they want to. Constantly changing the time the system is turned off risks patients losing trust in the online route, driving more demand through the telephone route which is less efficient to manage.
Taken to the limit, turning off online access completely would return to purely telephone access, with none of the flexibility for both patients and staff to use the efficiency of messaging and workflow.
Are there other advantages in cutting hours? Some take the view that they feel more in control if they know that no new requests can arrive after a certain time. Others turn off access at weekends, on the basis that some issues may have self limited by Monday, or they don’t want to see requests stored from the weekend, adding to a busy Monday.
Our usual advice to practices has been to keep online access open all the time, both in-hours and for OOH times when the message to patients sets a different expectation. However, we are clear that practices may turn off access themselves, either routinely or ad-hoc for example in the case of staff absence.
Based on the new data, we would suggest:
1. Reducing access hours has very little effect on total demand.
2. Practices may choose to limit hours, and it’s better to have consistent times so patients can be confident that online is open.
3. Whatever the decision, it should be up to the practice to determine access hours, and easily controlled by practice staff.
- Published in Evidence
Patient preferences and clinicians’ choices in 2020
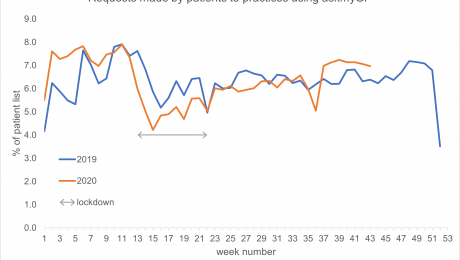
Perhaps surprisingly, latest figures from askmyGP showing patient contact activity are consistent with those from the equivalent period in 2019. Data show similar volumes of demand by patients, at approximately 6% of the practice list size making a request per week.
When offered a choice of ways to talk to their GP, 12% of patients expressed a preference for a face-to-face appointment, 34% preferred to be contacted by secure message and 50% by phone. Despite the obvious changes in methods of communication clinicians have continue to deliver care to their patients at a similar rate despite the effects of Covid.
Comparisons between years
Overall volumes of activity, expressed as percentage of the practice list making a request of their GP practice, are very similar when the same week is compared between 2020 and 2019. For example, the effects of the Christmas and Easter breaks can be observed in both years (Easter was slightly earlier in 2020), alongside e.g. public holidays in early and late May. Activity throughout the summer is nearly identical between years.
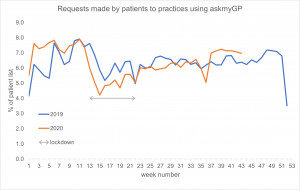
Communication methods
While similar proportions of cases were resolved, the mechanisms used to do so have changed substantially between years. Compared to 2019, responses to patients made less use of face-to-face and more use of secure messages and telephone consultation – the effects of Covid precautions being the most obvious explanation. Visits dropped from 0.92% to 0.53% and video usage remained low at 0.33% (not shown).
The askmyGP data is drawn from practices with diverse patient populations receiving a total of 4,067,068 patient requests during the year to date. The data illustrates patient contact by clinical episode, with video consultation and secure messaging with the patient’s usual NHS GP offered at no extra cost to either the practice or the patient.
Clinical judgement always takes precedence, meaning in some cases simple queries might be addressed by a quick answer by phone or message, while more complex presentations will warrant a face-to-face appointment, even in cases where this has not been requested by the patient. Practices are not bound by their patients’ contact preferences, but they use the information to guide their responses to patients.
Recent analysis by The Health Foundation similarly found that consultation rates changed only slightly – at askmyGP practices activity decreased by less than 1% between 1 March–30 June 2020, compared to the same period in 2019. However, they found there has been a dramatic swing away from face-to-face consultations. Between 1 March–30 June 2020, 8.5% of appointments were held face-to-face, compared to 38% during the same period in 2019. Use of remote consultation methods increased. Telephone appointments increased from 39% to 51%, online message from 23% to 40% and although video increased 50-fold, it remained low at 0.5%.
3 November 2020
- Published in Evidence
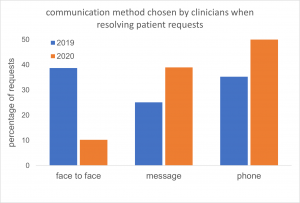
Celebrating five million patient requests
Five million patient milestone reached by online consultation and workflow system askmyGP
Five million patient requests have been managed by GP practices using the askmyGP online consultation and workflow system since September 2018. The system is used by practices throughout the UK with a combined list size of over 2 million patients. Clinicians at the practices use the system’s online triage tools to prioritise and deliver care by secure message, telephone, video or face-to-face appointment.
In those requests, 70% of patients chose to contact their GP online via the practice website, while the remaining patients phoned their practice. Half of patient requests were completed by the practice in two hours or less, including requests made online outside normal surgery hours.
Overall, patients asked for face-to-face appointments in only 12% of cases. 50% of patients asked to be contacted by the practice by phone and 34% asked for a secure message from their clinician. This pattern has varied considerably due to lockdown, with a clear shift away from face-to-face activities.
Across those patient requests, clinicians decided to see 12% of patients face-to-face. 86% of patients’ requests were resolved on the same day they contacted the practice. Recent patterns differ somewhat and can be explored in the live data presented on our website.
Across the five million patient requests, between 5% and 7.5% of patients on the practice list made contact each week; we observed that seasonal fluctuation is greater than the changes observed during lockdown. Patterns of demand in 2020 have remained similar to 2019 – this point is discussed further in our blog: patient preferences and clinicians’ choices in 2020
The five millionth patient request was received by the St John’s Medical Centre in Altrincham, early one Thursday in October 2020. St John’s has been using askmyGP to manage all of its patient requests since January this year. The request was closed by telephone 51 minutes later. GP partner Dr Marik Sangha said:
“With askmyGP we are simply getting through the work more efficiently. Although we are supporting the same numbers of patients, most don’t need to come into the surgery – you don’t need to physically see them. Nearly 80% of our patients make their request online, freeing up phone capacity for our more vulnerable patients who need more help. Patient feedback has been extremely positive.”
Harry Longman, chief executive of Salvie Ltd, the company behind askmyGP, said:
“This is a major milestone, and we are delighted that askmyGP continues to enable patients to get help promptly from their own GP. Despite the challenges presented by the Covid pandemic practices are able to understand, predict and manage patient demand much more flexibly, putting them in control of who they see and when, and ensuring patients receive appropriate support despite challenging circumstances.”
3 November 2020
- Published in Evidence
Contact Patient preferences and clinicians’ choices in 2019
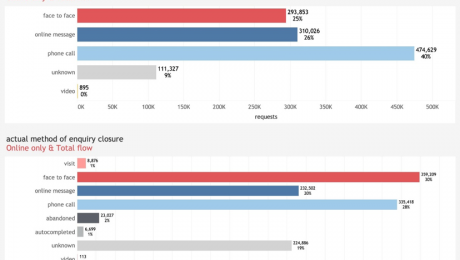
The 2019 full year figures from askmyGP reporting patient contact preferences show that when offered a choice of ways to engage with their GP Practice, 25% of patients expressed a preference for a face-to-face appointment, 26% asked to be contacted by secure message and 40% by phone. Data show continued low demand among both patients and clinicians for video consultations (0.08%).
Clinical judgement always takes precedence, meaning in some cases simple queries might be addressed by a quick answer by phone or message, while more complex presentations will warrant a face-to-face appointment, even in cases where this has not been requested by the patient. Practices are not bound by their patients’ contact preferences, but they use the information to guide their responses to patients.
The flow diagram illustrates the transitions between these ‘requested’ and ‘actual’ methods of delivery, indicating that the greatest shift was for patients who had asked for a phone call, but clinicians decided that a face-to-face appointment was needed. The result of these transitions was that clinicians resolved 30% of enquiries face-to-face, 20% via message and 28% by phone. In each case, clinicians were able to make use of the clinical presentation and medical history when selecting how best to address the patient’s needs.
The askmyGP data is drawn from practices with diverse patient populations receiving a total of 1.2 million patient requests during the period. The data illustrates patient contact by clinical episode, with video consultation with the patient’s usual NHS GP offered at no extra cost to either the practice or the patient. Unknown refers to cases where the preference was not recorded, even though help was provided to the patient.
25 February 2020
- Published in Evidence
Celebrating one million patient requests
One million patient milestone reached by online consultation and workflow system askmyGP
One million patient requests have been managed by GP practices using the askmyGP online consultation and workflow system since September 2018. The system is used by practices across the UK with a combined list size of 545,485. Clinicians at the practices use the system’s online triage tools to prioritise and deliver care by secure message, telephone, video or face-to-face appointment.
64% of patients chose to contact their GP online via the practice website, while the remaining patients phoned their practice. Half of patient requests were completed by the practice in two hours or less, including requests made online outside normal surgery hours.
Patients asked for face-to-face appointments in only 25% of cases. 45% of patients asked to be contacted by the practice by phone and 30% asked for a secure message from their clinician.
On reviewing patient requests, clinicians decided to see 37% of patients face-to-face. 88% of patients who needed an appointment attended the practice on the day they contacted the practice.
Across the one million patient requests, 6.5% of patients on the practice list made contact each week.
The one millionth patient request was received by the Concord Medical Centre in Bristol, which has been using askmyGP to manage all of its patient requests for more than two years. Senior partner Dr Simon Bradley said: “With askmyGP we are getting through the work more efficiently and continuity of care has improved too, with more patients consulting with their preferred GP. There are days where all outstanding consultations have been completed by 5.30pm, allowing the duty GP to manage urgent problems and process late requests that otherwise would have been passed forward to the following day.”
Harry Longman, chief executive of GP Access Ltd, the company behind askmyGP, said: “This is a major milestone and we are delighted that askmyGP has enabled a million patients to get help sooner from their own GP. That’s only possible by making it easier for practices to understand, predict and manage patient demand much more flexibly, putting them in control of who they see and when, managing their resources appropriately for each patient.”
- Published in Evidence
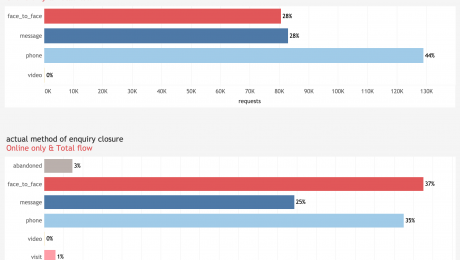
Patient preferences and clinicians’ choices in Q3 2019
The latest figures from askmyGP reporting patient contact preferences are consistent with those from earlier in the year. Data show continued low demand among patients for video consultations (0.06%).
When offered a choice of ways to talk to their GP, 27% of patients expressed a preference for a face-to-face appointment, 28% preferred to be contacted by secure message and 44% by phone. Slightly more patients asked for a face-to-face appointment than in previous months, but clinical decisions and actual method of delivery remain consistent.
The askmyGP data is drawn from practices with diverse patient populations receiving a total of 308,000 patient requests during the period. The data illustrates patient contact by clinical episode, with video consultation with the patient’s usual NHS GP offered at no extra cost to either the practice or the patient.
Clinical judgement always takes precedence, meaning in some cases simple queries might be addressed by a quick answer by phone or message, while more complex presentations will warrant a face-to-face appointment, even in cases where this has not been requested by the patient. Practices are not bound by their patients’ contact preferences, but they use the information to guide their responses to patients.
13 November 2019
- Published in Evidence
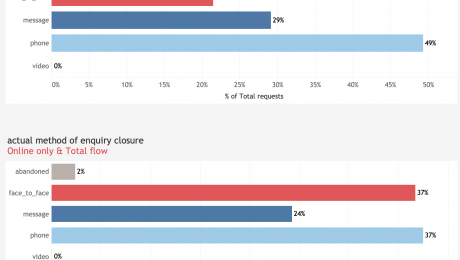
Latest figures continue to show low demand for GP video consultations
The latest figures from askmyGP reporting patient contact preferences show there has been no change in the low demand among patients for video consultations.
The askmyGP data for the second quarter of 2019 is drawn from practices with diverse patient populations receiving a total of 220,000 patient requests during the period. The data illustrates patient contact by clinical episode, with video consultation with the patient’s usual NHS GP offered at no extra cost to either the practice or the patient.
When offered a choice of ways to talk to their GP, 21% (Q1 25%) of patients expressed a preference for a face-to-face appointment, 29% (Q1 28%) preferred to be contacted by secure message and 49% (Q1 47%) by phone. Patients requested a video consultation in less than 0.1% (Q1 0.1%) of cases.
While practices are not bound by their patients’ contact preferences, they use the information to guide their responses to patients. Clinical judgement always takes precedence, meaning in some cases simple queries might be addressed by a quick answer by phone or message, while more complex presentations will warrant a face-to-face appointment, even in cases where this has not been requested by the patient.
13 August 2019
- Published in Evidence
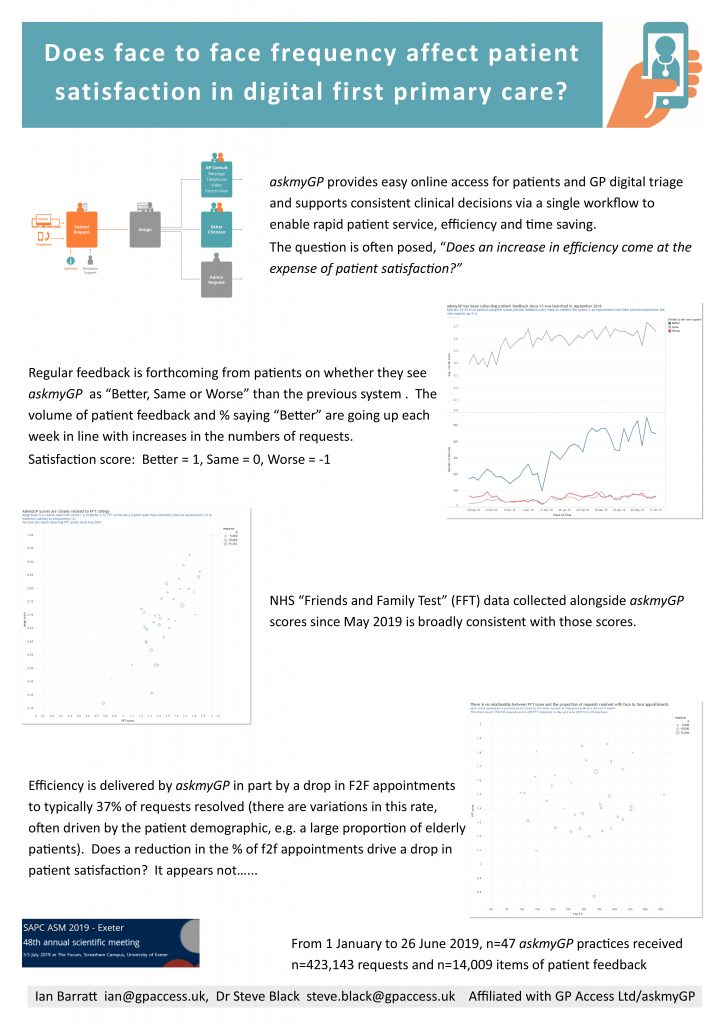
Does F2F frequency affect patient satisfaction in digital first primary care? SAPC Exeter ASM poster
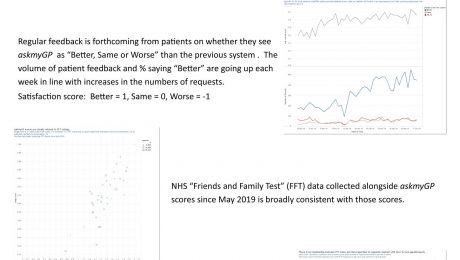
Many have wondered whether patient satisfaction is affected by their chance of seeing a GP face to face. The study done for the Exeter Annual Scientific Meeting of SAPC (Society for Academic Primary Care) analysed 14,009 patient feedbacks from 423,143 episodes managed through askmyGP from 1 January to 26 June 2019.
Presented by Ian Barratt and Steve Black at the conference. Download pdf here.
- Published in Evidence
- 1
- 2